Colon / Rectum Cancer
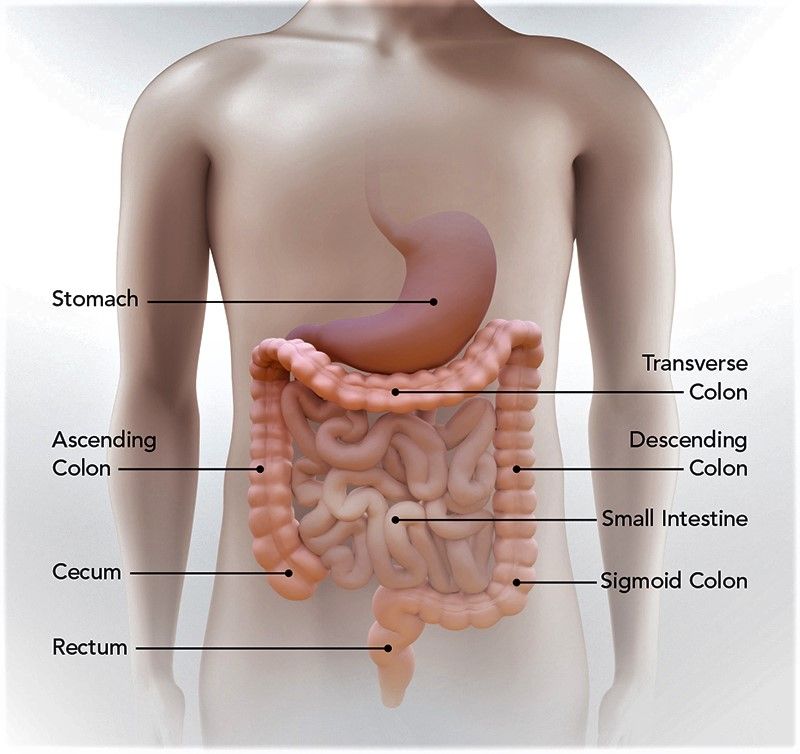
Colorectal cancer is a disease in which cells in the colon or rectum grow out of control. Sometimes it is called colon or even bowel cancer, for short.
The colon is the large intestine or large bowel. The rectum is the passageway that connects the colon to the anus.
Sometimes abnormal growths, called polyps, form in the colon or rectum. Over time, some polyps may turn into cancer. Screening tests can find polyps so they can be removed before turning into cancer. Screening also helps find colorectal cancer at an early stage, when treatment works best.
Symptoms of Bowel Cancer
The 3 main symptoms of bowel cancer are:
- persistent blood in your poo – that happens for no obvious reason or is associated with a change in bowel habit
- a persistent change in your bowel habit – which is usually having to poo more and your poo may also become more runny
- persistent lower abdominal (tummy) pain, bloating or discomfort – that's always caused by eating and may be associated with loss of appetite or significant unintentional weight loss
Most people with these symptoms do not have bowel cancer. Other health problems can cause similar symptoms. For example:
- blood in the poo when associated with pain or soreness is more often caused by piles (haemorrhoids)
- a change in bowel habit or abdominal pain is usually caused by something you've eaten
- a change in bowel habit to going less often, with harder poo, is not usually caused by any serious condition – it may be worth trying laxatives before seeing a GP.
These symptoms should be taken more seriously as you get older and when they persist despite simple treatments.
When to get medical advice?
See a GP If you have any of the symptoms of bowel cancer for 3 weeks or more.
The GP may decide to:
- examine your tummy and bottom to make sure you have no lumps
- arrange for a simple blood test to check for iron deficiency anaemia – this can show whether there's any bleeding from your bowel that you have not been aware of
- arrange for you to have a simple test in hospital to make sure there's no serious cause of your symptoms
Make sure you see a GP if your symptoms persist or keep coming back after stopping treatment, regardless of their severity or your age. You'll probably be referred to hospital.
Causes of Bowel Cancer
The exact cause of bowel cancer is not known, but there are a number of things that can increase your risk, including:
- age – almost 9 in 10 people with bowel cancer are aged 60 or over
- diet – a diet high in red or processed meats and low in fibre can increase your risk
- weight – bowel cancer is more common in overweight or obese people
- exercise – being inactive increases your risk of getting bowel cancer
- alcohol – drinking alcohol might increase your risk of getting bowel cancer
- smoking – smoking may increase your chances of getting bowel cancer
- family history – having a close relative (mother or father, brother or sister) who developed bowel cancer under the age of 50 puts you at a greater lifetime risk of developing the condition; screening is offered to people in this situation, and you should discuss this with a GP
Some people also have an increased risk of bowel cancer because they've had another condition, such as extensive ulcerative colitis or Crohn's disease in the colon for more than 10 years.
Although there are some risks you cannot change, such as your age or family history, there are several ways you can lower your chances of developing the condition
COLON and RECTUM CANCER DATA Period 2019 -2024
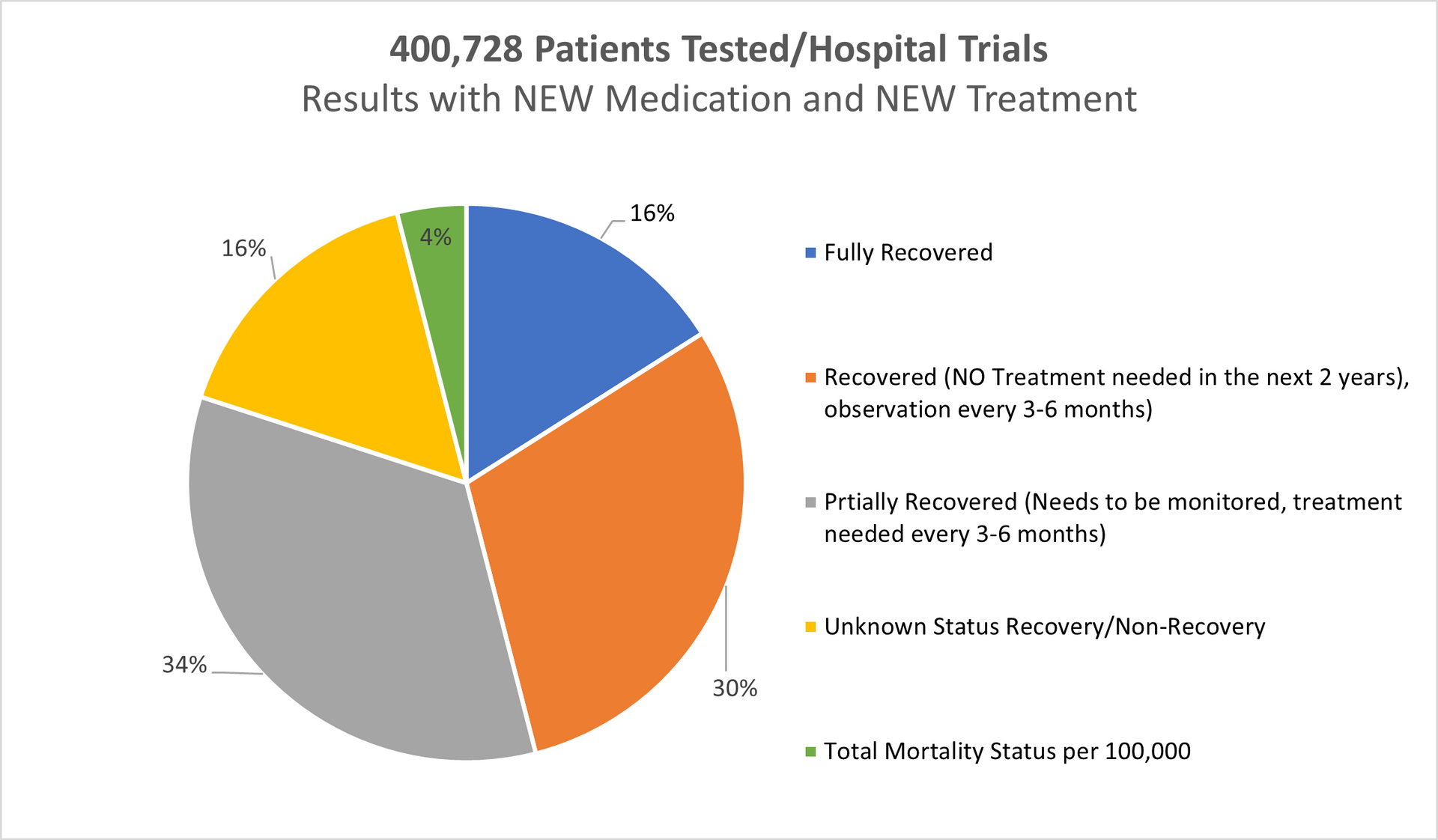
Hospital Trials and Treatment with our NEW Medication
Mortality in EU 2019-2024: 269,994; (EU hospitals Standard Treatment)
Mortality in the UK 2019-2024: 62,834 (UK hospitals Standard Treatments)
Result using our New Medication/Treatment (Testing period 2019-2024 all age groups):
Tested patients in UK, Switzerland, Germany and Italy: 400,728
Fully recovered: 16%
Recovered (No treatments needed in the next 2 years monitoring every 6 months): 30%
Partially Recovered (Further treatments needed as precaution after 3-6months passed): 34%
Unknown Recovery/ Non-recovery: 16%
Deaths in Total: Less than 4% (The highest % in the group 56-65).
REFERENCES TO THE DATA ABOVE (Period 2019-2024):
Age Gap: The youngest person was 16 years of age
The oldest person was 88 years of age
Gender:
Female: 176,322 of 400,728
Male: 224,406 of 400,728
Age group 16-25 > 1.4%
Age group 26-45 > 29.9%
Age group 46-65 > 40.6%
Age group 66-90 > 28.1%
---------------------------------
Total: 100%
========================
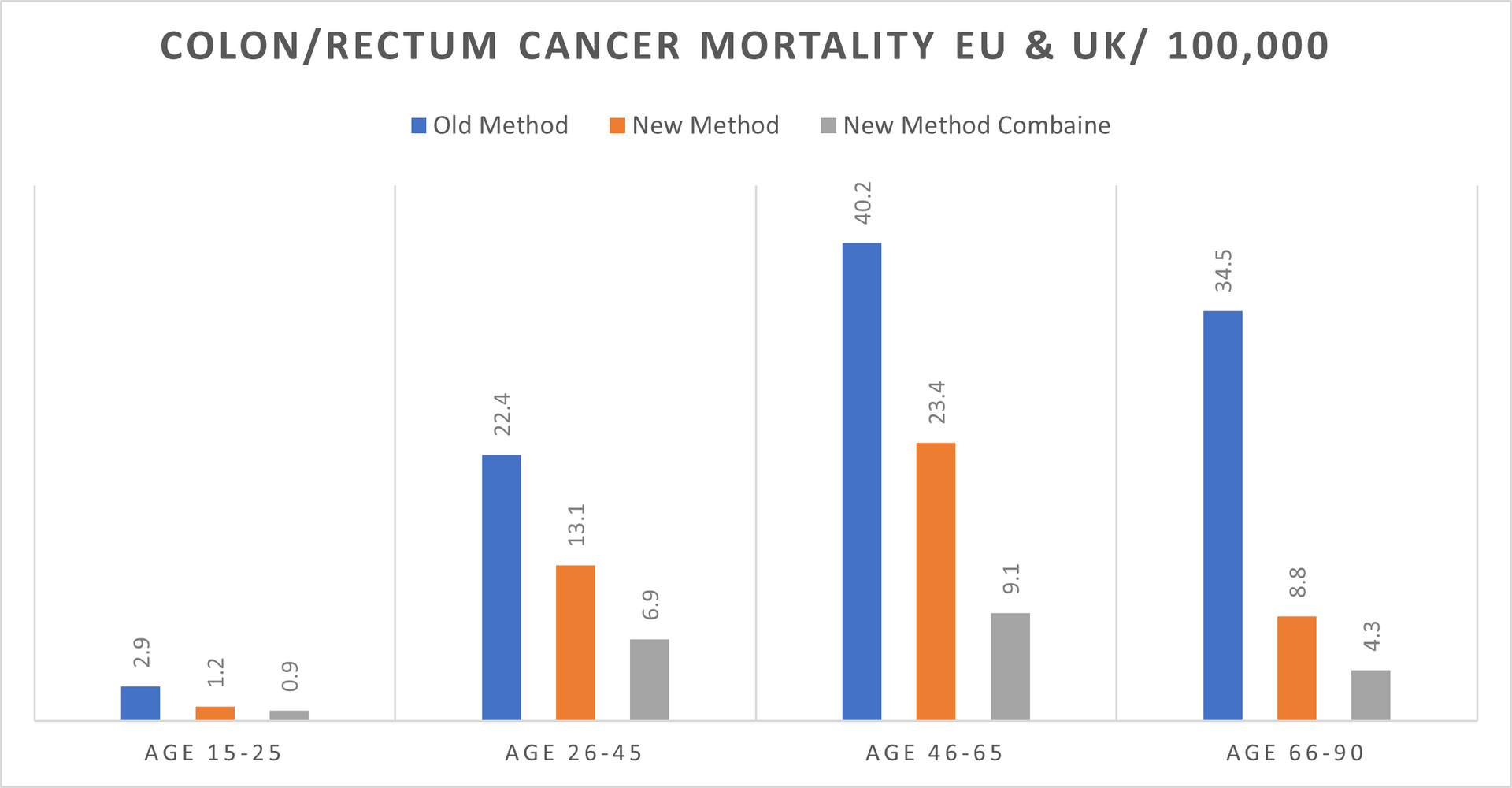
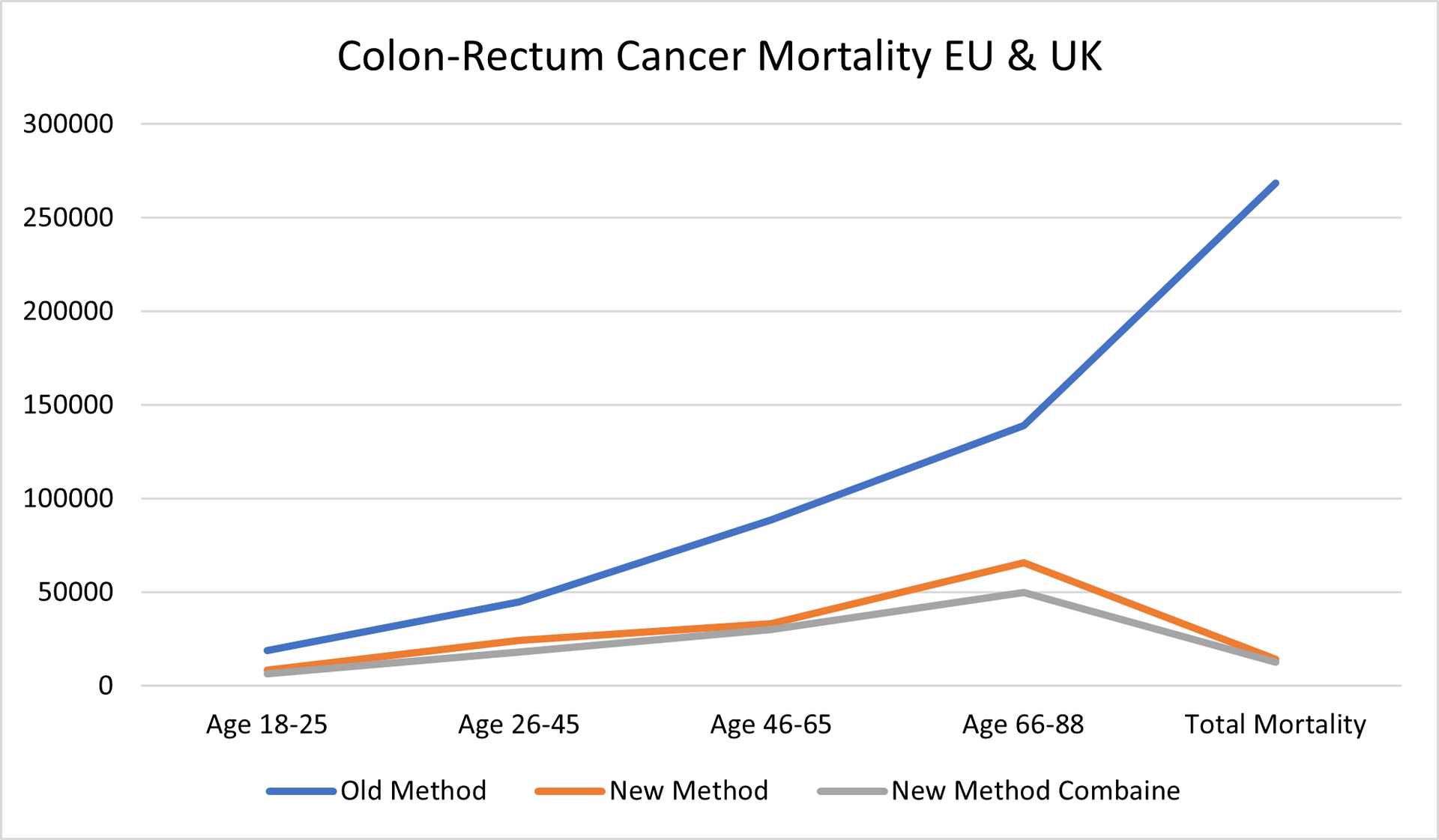
Methods:
Old Methods meaning the STANDARD METHODS used by the hospital on a daily basis for the last minimum 5 years in Europe and in the United Kingdom.
New Methods meaning our NEW MEDICATION/TREATMENT with which we came out after over 14 years of research and tests.
New Methods Combine meaning our NEW MEDICATION/TREATMENT COMBINED in double parallel treatment > NEW MEDICATION and different way of treatment combined with chemotherapy or combined with radiotherapy or combined with chemo and radiotherapy.
Separately we tested our NEW MEDICATION combined with "OLD" methods used by the hospitals in Europe and in the United Kingdom however, the final readings cannot be 100 percent accurate and cannot be as such used for whatever comparison.
Mortality:
In the Europe 2019-2024 > 19.2%
In the United Kingdom 2019-2024 > 14.4%
With our NEW Medication/Treatment in Europe & United Kingdom 2019-2024 > Just above 4%.
The % of "Unknown Recovery / Non-Recovery" dropped (2018/23 was 18%) to 16% mainly in the age group 26-45 which we believe has not increased due to different culture in preparing the food not to mention that this age group swing in majority to organic food.
There is an increase of mortality in Europe for 5.1% while in the UK mortality went up by 2.1%.
All patients being chosen randomly what also might be the point of just above 4% mortality rate.
OUR RESEARCH and MORTALITY DATABASE 2019-2024
Cancer is one of the biggest health challenges worldwide. Since starting the research in 2011/12, the percentage of all deaths from cancer has risen from 9.6% in 2011 to 14.9% 10 years later; in the last 5 years this has risen again to where we now have 16.2% of all deaths recorded as cancer deaths.
Taking into consideration that in the period 2019-2024 the average European and the United Kingdom population was 760.3 million, an average 4,880,664 new cases were reported yearly during the same period. This is an ASR of 280, and a cumulative risk of 29.8%.
Breast, Colorectum, and Lung cancers were the most common cancers across both sexes.
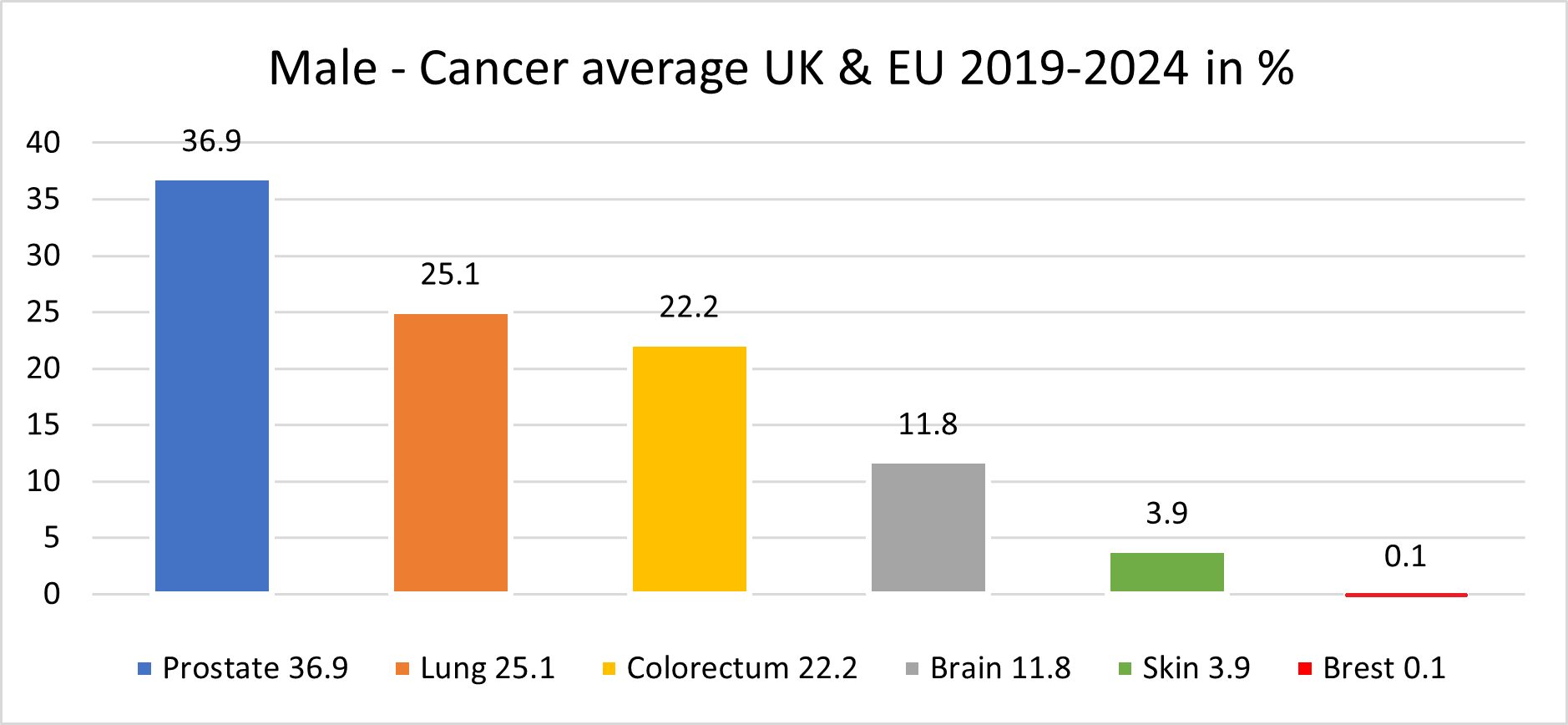
The male population in this period, some 370.2 million, recorded an average of 2,482,117 new cancer cases per year; an ASR of 321.4 per 100,000 and a cumulative risk of 33.1%.
The top 3 most common cancers among males were Prostate, Lung, and Colorectum cancer.
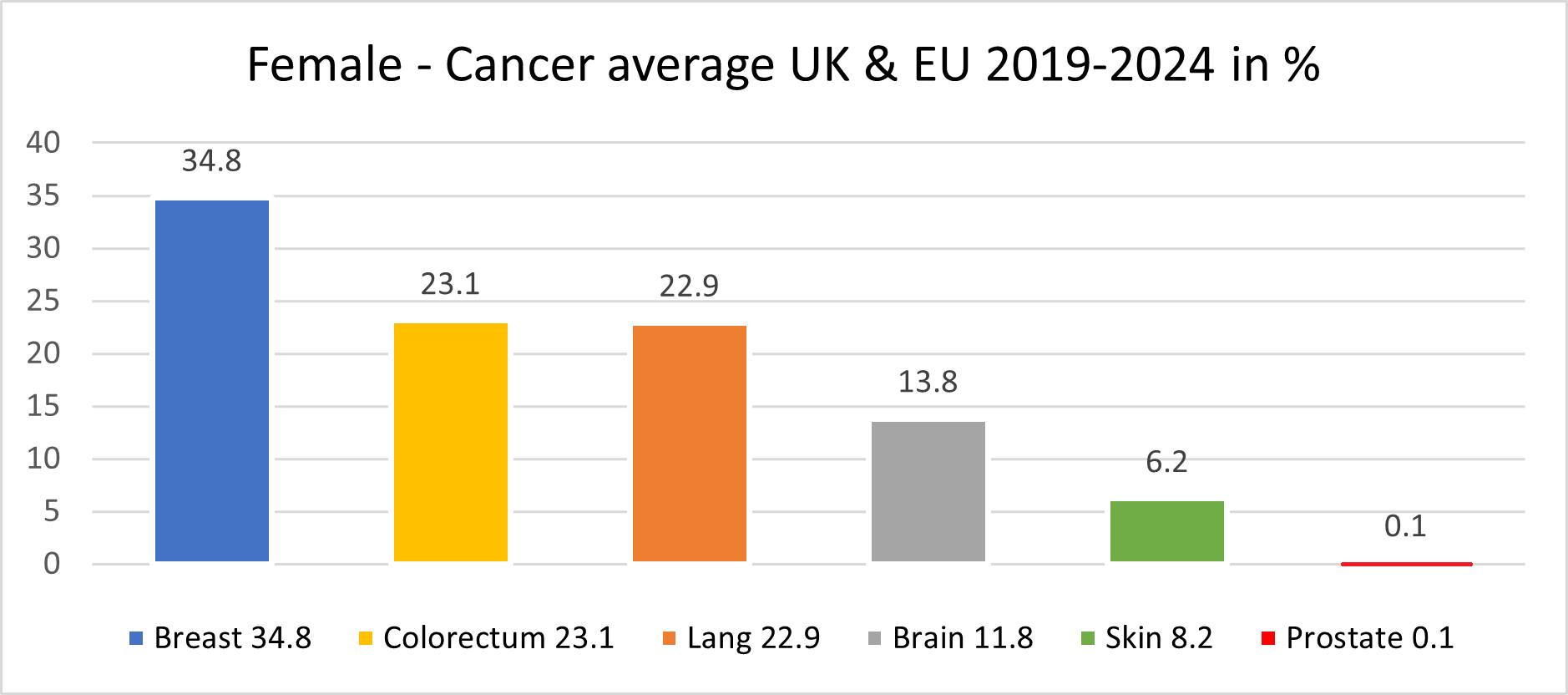
The female population in this period, some 390.1 million, recorded an average 2,398,547 new cancer cases per year; an ASR of 258.6 and a cumulative risk of 26.5%.
The top 3 most common cancers in females were Breast, Colorectum, and Lung cancer.
A significant point with cancer in the female population was the drop in lung cancer to 3rd place, with colorectum cancer overtaking the 2nd place.
Our mortality database is a collection of death registration data which includes cause of death information from member states; we use only the data which has been properly coded to the International Classification of Diseases (ICD).
What has also changed in recent years is the age of the death rate. This had declined over time in several countries due to life improvements, early diagnoses, medical advances, and a general reduction in risk factors like smoking and even drinking. However, there is a worrying emerging trend with rates of cancer in the population group aged up to 16.
This is rising well over expectations, especially in the United Kingdom, Spain and France.
PERIOD 2018 -2023
COLON and RECTUM CANCER DATA
Colon and Rectum Cancer Data
Mortality in EU 2018-2023: 268,428; Mortality in UK 2018-2023: 40,483 (EU & UK Standard Treatments)
Result by Starting using our New medication (Testing period 2018-2023 all age groups):
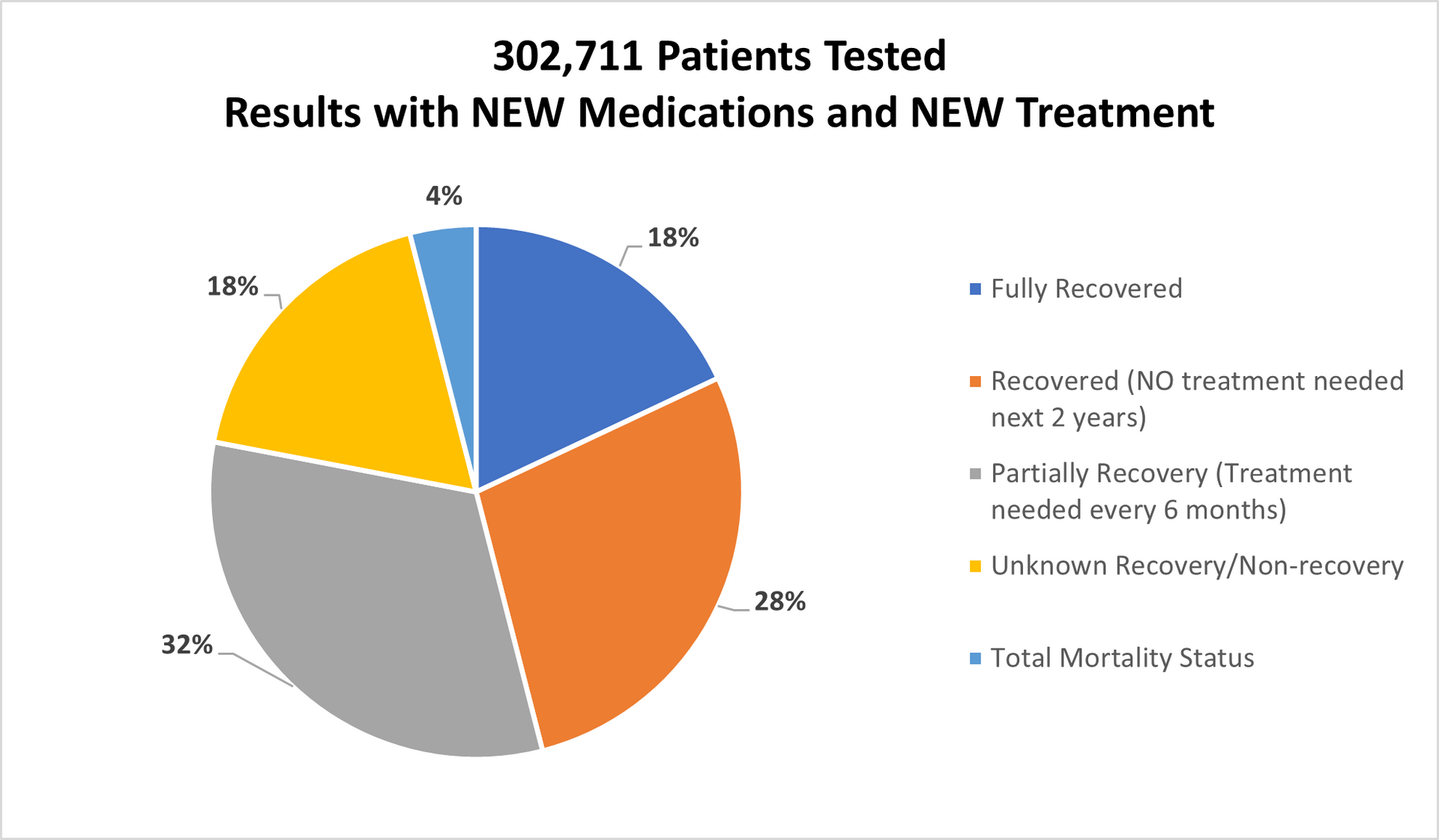
Tested patients in UK, Switzerland, Germany and Italy: 302,711
Fully Recovered: 18%
Recovered (No further treatments needed for period of next couple of years): 28%
Partially Recovered (Further treatments needed as precaution after 6months passed):32%
Unknown Recovery/ Non-recovery: 18%
Deaths in total: 4% (Mostly people age over 58).
REFERENCES TO THE DATA ABOVE:
Age Gap:
The youngest person was of 18 years of age
The oldest person was well over 88 years of age
Gender:
Female: 101,283 of 302,711
Male: 201,428 of 302,711
- % of age group 18-25 was 1.4%
- % of age group 26-45 was 22.2%
- % of age group 46-65 was 48.9%
- % of age group 66-88 was 27.5%
Methods:
Old Methods meaning the standard methods used by hospital on daily basis for last minimum 5 years in EU and in the UK.
New Methods meaning our medication/treatment with which we came out after over 12 years of research and test.
New Methods combine meaning our medication/treatment combined in double parallel treatment > new medication and different way of treatment
Separate there are also results of our new medication/treatment combined with "old" methods however the final readings cannot be 100 percent accurate and cannot be as such used for whatever compares.
Mortality:
In the Europe 2018-2023 > 19.8%
In the United Kingdom 2018-2023 > 11.2%
With our medication/treatment in Europe & United Kingdom 2018-2023 > 4.4%.
The % of "Unknown Recovery / Non-Recovery" nearly the same (2017/22 > 15%).
There is increase of mortality in Europe for 2.7% while in UK mortality gone up by 1.1%.
All patients being chosen randomly.
