Prostate Cancer
Age seems to be be the most important risk factor for the prostate cancer. With young people, the prostate cancer is quite rare but we cannot take it for granted. Normally are diagnosed with age 60 or even more after age 65.
There's a good chance of recovery if it's detected at an early stage. For this reason it's vital that man check possibility of having prostate cancer regularly.
Symptoms of Prostate Cancer
Prostate cancer is a tumour disease that is usually causes symptoms at a late stage. There are three stages
- Early Stage
Normally we would fins prostate cancer located at the back of prostate, where there are no any critical organs.
The tumour does not cause any symptoms or will give a signal that something is wrong. Symptom might remain silent not just years but decades.
- Late Stage
Only when comes to a significant increase in size does make the tumour cause symptoms. There are coming problem with urinating, blood in the urine and incontinence.
- B-Symptoms in Cancer
In case the cancer progress, B-Symptoms can occur. The B-Symptoms include night sweats, fiver and weight loss.
Causes of Prostate Cancer
The exact causes of prostate cancer are not fully discovered simply because there are so many factors known to increase the risk of prostate cancer.
These include:
- age – the risk increases as you get older
- a family history of prostate cancer
- a previous diagnosis of prostate cancer
- genetic changes
- being tall
- being overweight or obese
- drinking alcohol
- smoking
- origin
- taking medications or supplements
Diagnosing Prostate Cancer
Whenever we are diagnosing prostate cancer we have to examine various techniques most probably as combination of all possible ways:
- PSA Value
- PSMA-PET
- Palpation Examination
- MRI
- DNA (we are the only one)
- Tissue Sampling
When come to Late Stage
With a significant increase in size does the tumour cause the Symptoms where problems starts like:
- Urinating problems, blood in the urine and incontinence – The urethra, through which urine flows from the bladder, is surrounded by the prostate gland in a circle. Because of the increase in the size of the tumour within the prostate with an increase in pressure within the prostate surrounded by a rigid capsule, compression of the urethra can occur. The urine can no longer drain through the compressed urethra and accumulates upwards into the urinary bladder and from there via the ureter to the kidneys. Once you cannot urinate despite a full bladder and urge to urinate we come to so called urinary retention. Normally is painful and unpleasant for the person affected. While urinary tract infections are very common in women due to the short urethra and the close relationship between the urethra and the anus, urinary tract infections in men are very rare. However, if urine is prevented from draining, the stagnant urine offers an ideal nutrient medium for bacteria. This can lead to repeated urinary tract infections. In case where the tumour start growing into urethra normally come to injure it. This can lead to blood in urine.
- Erectile Dysfunction – Blood flow to the penis is important to get and maintain erection. The tumour can also grow into the blood vessels, most common to those that supply the penis with blood and oxygen. Once this happen, the ability to achieve an erection can become slimer.
- Fractures and Bone Pain - In majority of the man, the tumour is detected when has already spread. It is quite normal that the tumour spread to bones on the back [vertebral body], there are quite a few patients present with acutely painful back problems. Once the tumour grows, normally destroying the bone. This is very serios injury and lead to bone fractures. If come to "unclear" fractures, cancer should be and must be considered.
- Spinal Cord - Once growth in the spine, there always will be a risk of a spinal cord. When the posterior edge of a vertebral body is fractured, the vertebral body can press on the spinal cord, which is surrounded by the vertebral bodies, destroying the long nerve conductions that extend from the brain through the spinal cord into the organs.
MRI Screening
T2W Images
- Hypointense lesions in the peripheral zone. Hyperintense lesions in the transition zone.
DWI (Diffusion Weighted Imaging)
- Area within limited diffusion shows high-signal intensity
DCE (Dynamic Contrast Enhanced)
- Early enhancement and rapid leaching are observable
Spectroscopy
- Decrease in citrate peak and increase in choline peak
T1W Images
- After the administration of the contrast agent: enhancement of the lesion
Lymph Node
- Size and morphological changes of the lymph nodes

Treatment of Prostate Cancer
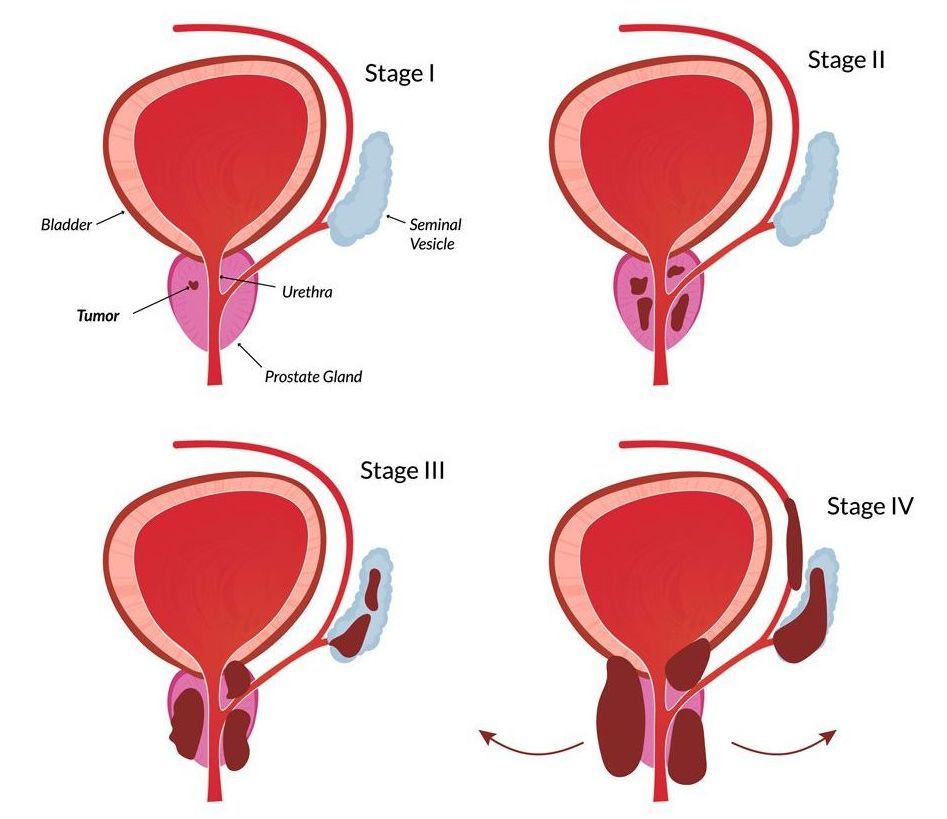
If cancer is detected at an early stage, it can be treated before it spreads to other parts of the body. Prostate cancer is treated using a depending the level:
1. Therapy for low risk level
T-Stage T1-T2a
Gleason Score ≤ 6
PSA Value < 10ng/ml
2. Therapy for medium risk level
T-Stage T2b
Gleason Score 7
PSA Value 10-20ng/ml
3. Therapy for high risk level
T-Stage ≥ T2c
Gleason Score 8-10
PSA Value > 20ng/ml
Low Risk Level Therapy
For patients at low risk, choosing the optimal therapy is a major challenge.
A wait-and-see therapy regimen can be considered. The prerequisite for this is that only two of the tissue samples taken were positive and that less than 50% of the tumour was measured in the removed tissue.
With this approach, an MRI examination should be considered, as this can rule out the possibility that there may already be a larger tumour in the prostate than would be apparent from other examinations.
With this approach, the PSA value is checked regularly. One MRT of the prostate can be done every six months to annually. Also, either in the event of an increase in values or a change or once a year, a biopsy of the findings should be taken to evaluate what the Gleason score is.
Low Risk - Radiation
Low risk patients has option of radiation therapy. In the low risk level, radiation therapy can be carried out from the outside as well as from the inside
Teletherapy
In the case of radiation therapy from the outside (teletherapy), a so-called planning CT is performed, on which the prostate is defined by the radio-oncologist.
A few days after planning, radiation therapy can usually begin. The patient is positioned on a table and irradiated from the outside with photons or protons.
The radioactive radiation that concentrates in the prostate causes damage to the DNA - the genetic material of tumour cells. With damage to the DNA, the tumour cells lose the opportunity to divide and perish consecutively.
The disadvantage of external radiation therapy is the exposure of radiogenic doses to the bladder, rectum and the heads of the hip.
Low Risk - Radiation
Brachytherapy
In the case of radiation from the inside, radioactive chains are implanted in the prostate via the perineal region. The perineal region is the area between the testicles and anus.
In order to be able to insert the radioactive parts precisely into the prostate, this is done under sonographic control. As with a tissue sample of the prostate, the sonography is carried out via the rectum and thus the prostate is shown.
The prerequisite for this procedure is that the prostate is not too large and that the patient does not have any sequelae of an enlarged prostate (problems urinating).
After these radioactive markers are implanted in the prostate, they will have the same effect as the radiation from the outside.
Low Risk - Surgery
At any stage including the early stages surgery can and could be considered. This can be as open surgery or as robotic surgery.
Low Risk - Watchful Waiting
In patients who have only a very short life expectancy, an active control approach can also be carried out, in which, however, no therapy would be carried out as the tumour increases, but only waiting for symptoms such as pain in order to then treat them symptomatically.
Medium Risk
For patients in the medium risk level, surgery or radiation therapy can be carried out externally.
Radiotherapy from the inside is reserved for higher-grade risk groups. However, there are also approaches in which radiation therapy from the outside is combined with radiation therapy from the inside.
If you decide to undergo radiation therapy, you can differentiate this middle stage into two other sub-risk groups (favorable and unfavorable).
Here there is the prognostically more favorable stage, in which less than half of the tissue biopsies collected were positive, which probably does not benefit from hormone therapy.
In the case of an intermittent stage of a higher risk group, short-term hormone therapy of about six months should be considered in addition to radiation therapy.
There is no data that this prolongs survival. However, there is data that this reduces the rate of metastases, which can have a direct impact on survival.
High Risk
For patients in the high risk stage, the question of surgery and radiation therapy arises again. In the case of radiation therapy, parallel hormone therapy should be carried out and hormone therapy should be given for a minimum period of two to three years.
The disadvantages of hormone therapy are the corresponding side effects (hot flashes, pain in the mammary glands, an increased risk of thrombosis and embolism, mood swings, loss of libido and erectile dysfunction).
Therapy for Metastatic Disease
In the case of metastatic disease, drug therapy is in the foreground. This is hormone therapy with chemotherapy and one of the new modern drugs (apalutamide or enzalutamide).
However, there are also data on the benefits of local radiotherapy of the prostate and irradiation of all metastatic foci in patients with fewer than five metastases.
Surgery in Prostate Cancer
Should you opt for surgery?
Surgery is very important component in the treatment of prostate cancer. However depending on your background you should consider of the alternative offered by radiotherapy.
Surgery itself can be performed in any stages which might prevent spreading.
In case if metastases are already present before the prostate surgery in which case we can have an unnecessary major operation, a PSMA-PET would be very suitable for high risk patients. With such procedure we can detect nearly 80-85% possible daughter foci.
If we are having localized prostate cancer, the patient often has to choose between surgery and radiotherapy. Both therapies has been compared all over again and again.
There was no difference between radiotherapy and surgery in terms of tumour control and overall survival.
This poses a great challenge for the patient as to whether he or she should opt for surgery or radiation therapy. There is one study named "English Protect Trial".
Radiotherapy v Surgery: Differences, Complication and Side Effect
The majority of the two procedures differ in terms of the range of complications.
In patients who are irradiated, erectile functionality can usually be preserved more often than after surgery. However, since patients at higher risk also need hormone therapy for radiation therapy, this will usually reduce erectile function at least for the period of hormone therapy (two to three years) after radiation therapy.
Hormone therapy is usually not necessary in low-risk patients and controversial in moderate-risk patients.
In patients who lose erectile function after radiation therapy, the drug approach with drugs such as Viagra or Cialis is more often more promising than after surgery.
A disadvantage of radiation therapy in high risk situations is that radiation therapy is carried out in combination with hormone therapy. Hormone therapy usually lasts two to three years.
However, if you decide to have surgery in a high-risk situation, you have to remember that radiotherapy may be necessary in patients with a larger tumour (via T3 breakthrough of the cancer through the prostate capsule or penetration of the cancer into the seminal vesicle) and in patients in whom a remnant remains in the prostate after surgery.
In the past, all patients with T3 or rest were irradiated after surgery. However, since not all patients will develop a recurrence in this situation, one waits today and checks the PSA value.
It is possibility that up to 50 percent of patients will develop a PSA recurrence, for which radiotherapy is necessary. The combination of both therapies modules is associated with the highest risk of complications, as the complications add up.
The aim of the operation is to remove the entire prostate, including relevant risk areas.
The operation can be used in all risk levels (low risk, medium risk and high risk), as an alternative to radiotherapy. While there might be speculation which way to go either radiotherapy or surgery because complications differs, cancer survival and tumour control appear to be comparable with both methods.
Read more about the Prostate cancer at Prostate cancer standard treatment low price Zdenko Kos Foundation
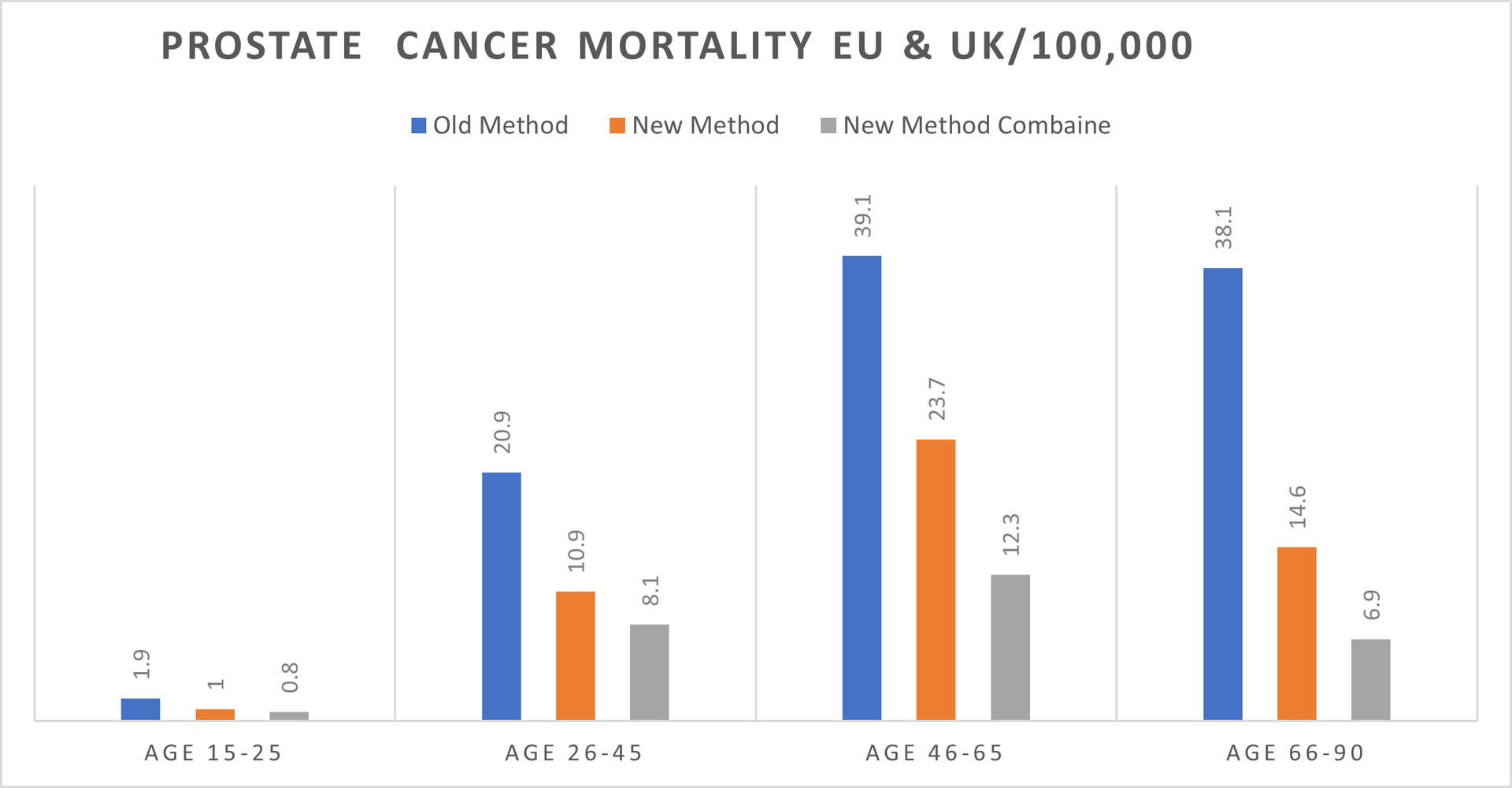
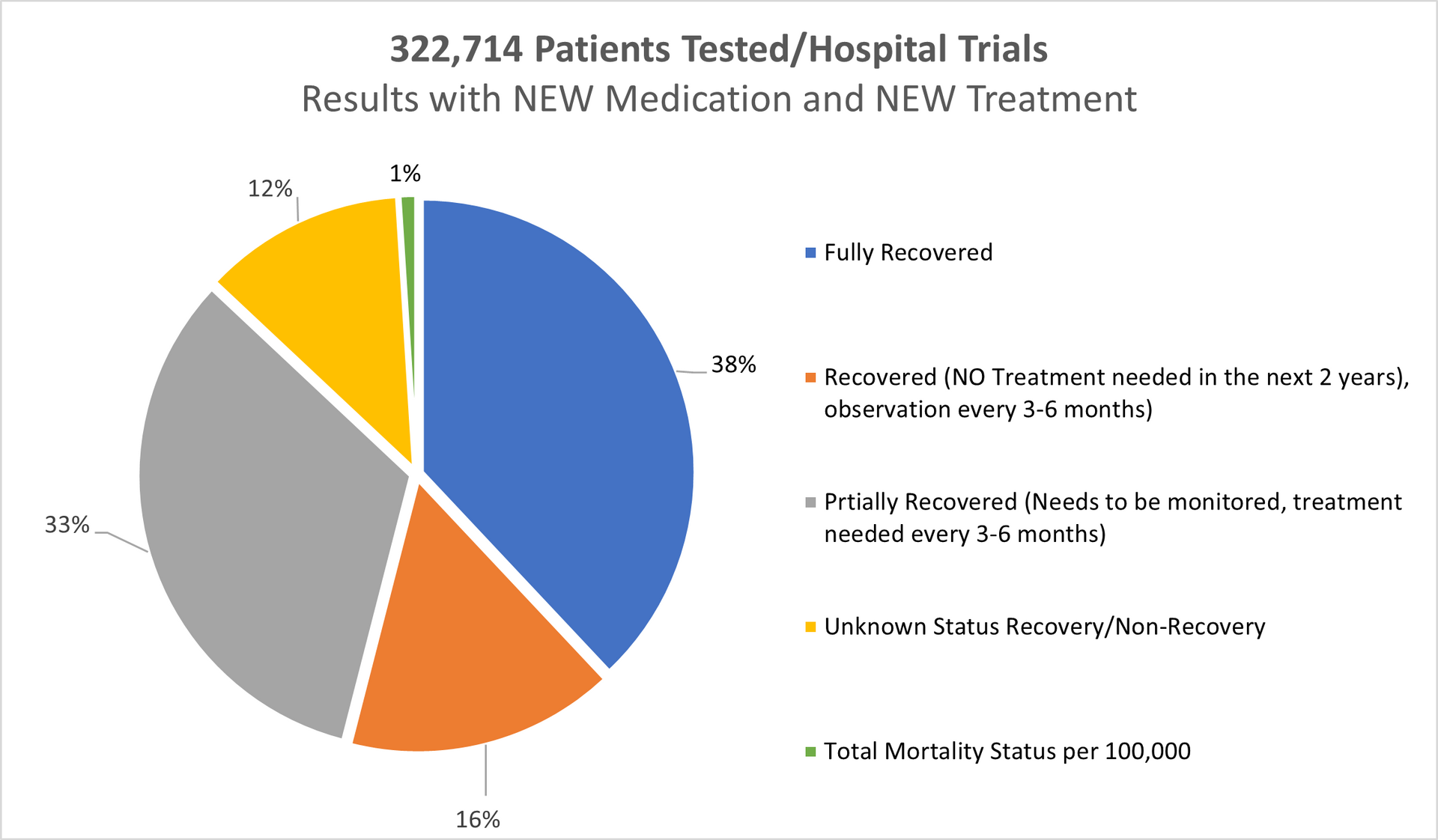
PROSTATE CANCER DATA Period 2019 -2024
Hospital Trials and Treatment with our NEW Medication
Mortality in EU 2019-2024: 40,833; (EU hospitals Standard Treatment)
Mortality in the UK 2019-2024: 21,872 (UK hospitals Standard Treatments)
Result using our New Medication/Treatment (Testing period 2019-2024 all age groups):
Tested patients in UK, Switzerland, Germany and Italy: 322,714
Fully recovered: 38%
Recovered (No treatments needed in the next 2 years monitoring every 6 months): 16%
Partially Recovered (Further treatments needed as precaution after 3-6months passed): 33%
Unknown Recovery/ Non-recovery: 12%
Deaths in Total: Less than 1% (The highest % in the group 46-65).
REFERENCES TO THE DATA ABOVE (Period 2019-2024):
Age Gap: The youngest person was not even 24 years of age
The oldest person was nearly 69 years of age
Gender:
Female: 6 of 322,714
Male: 322,708 of 322,714
Age group 16-25 > 0.9%
Age group 26-45 > 20.6%
Age group 46-65 > 52.3%
Age group 66-90 > 26.2%
---------------------------------
Total: 100%
====================
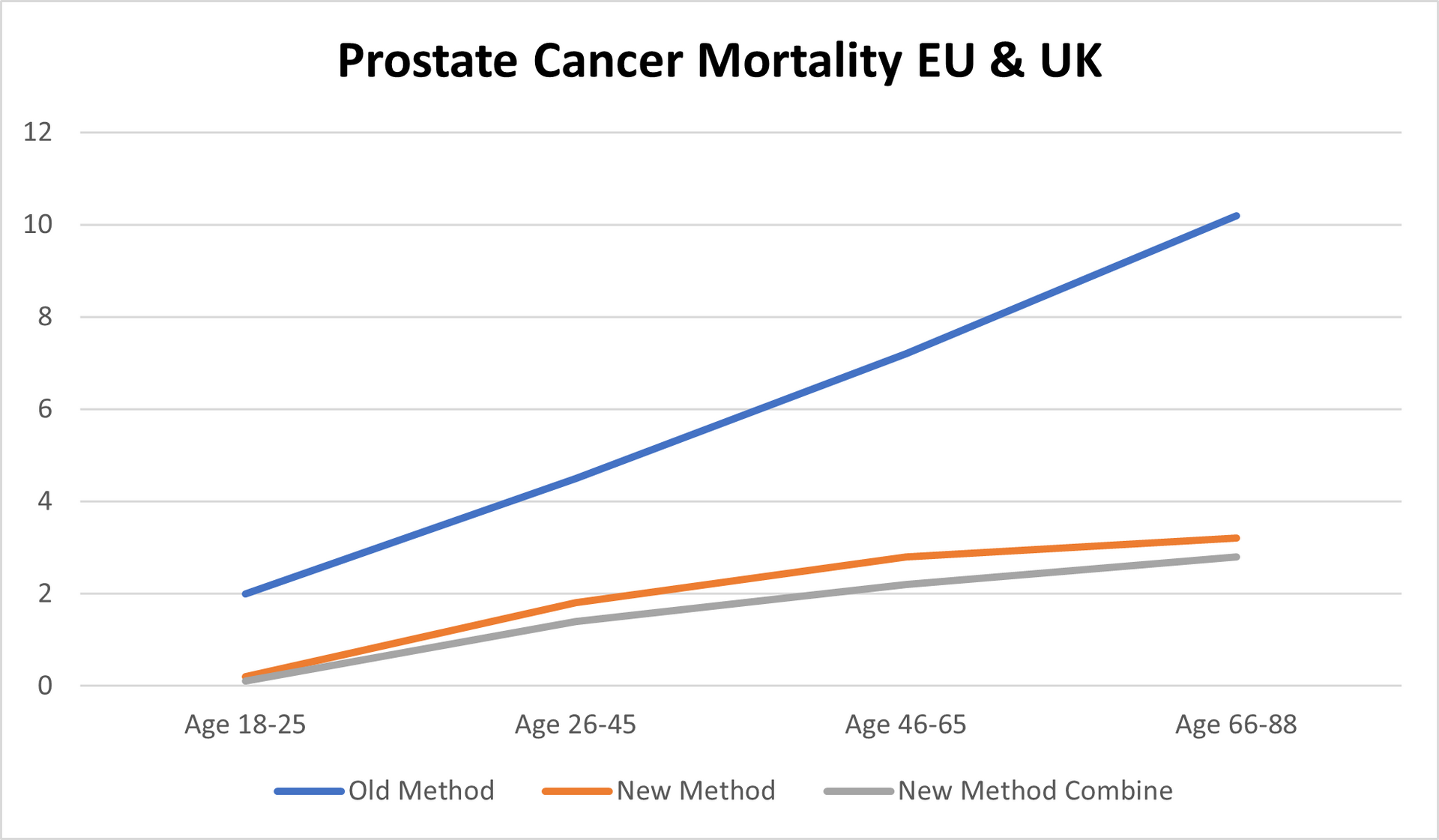
Methods:
Old Methods meaning the STANDARD METHODS used by the hospital on a daily basis for the last minimum 5 years in Europe and in the United Kingdom.
New Methods meaning our NEW MEDICATION/TREATMENT with which we came out after over 14 years of research and tests.
New Methods Combine meaning our NEW MEDICATION/TREATMENT COMBINED in double parallel treatment > NEW MEDICATION and different way of treatment combined with chemotherapy or combined with radiotherapy or combined with chemo and radiotherapy.
Separately we tested our NEW MEDICATION combined with "OLD" methods used by the hospitals in Europe and in the United Kingdom however, the final readings cannot be 100 percent accurate and cannot be as such used for whatever comparison.
Mortality:
In the Europe 2019-2024 > 26.8%
In the United Kingdom 2019-2024 > 17.1%
With our NEW Medication/Treatment in Europe & United Kingdom 2019-2024 > Just below 1%.
The % of "Unknown Recovery / Non-Recovery" dropped again (2018/23 was 18%) to 12% mainly in the age group 26-45 which we believe has 3 different reasons for.
There is an increase of mortality in Europe for 6.2% while in the UK mortality went up by 3.1%.
All patients being chosen randomly what also might be the point of just below 1% mortality rate.
OUR RESEARCH and MORTALITY DATABASE 2019-2024
Cancer is one of the biggest health challenges worldwide. Since starting the research in 2011/12, the percentage of all deaths from cancer has risen from 9.6% in 2011 to 14.9% 10 years later; in the last 5 years this has risen again to where we now have 16.2% of all deaths recorded as cancer deaths.
Taking into consideration that in the period 2019-2024 the average European and the United Kingdom population was 760.3 million, an average 4,880,664 new cases were reported yearly during the same period. This is an ASR of 280, and a cumulative risk of 29.8%.
Breast, Colorectum, and Lung cancers were the most common cancers across both sexes.
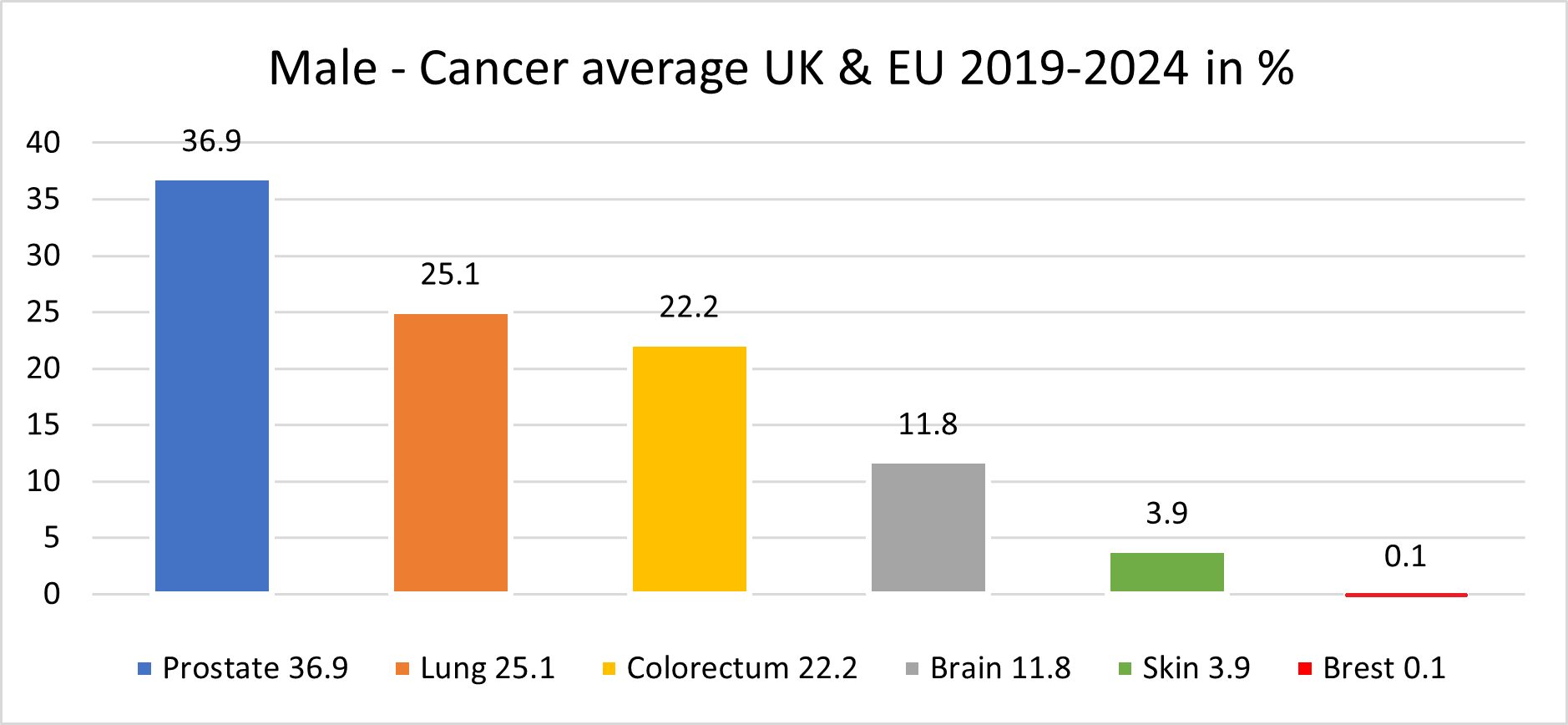
The male population in this period, some 370.2 million, recorded an average of 2,482,117 new cancer cases per year; an ASR of 321.4 per 100,000 and a cumulative risk of 33.1%.
The top 3 most common cancers among males were Prostate, Lung, and Colorectum cancer.
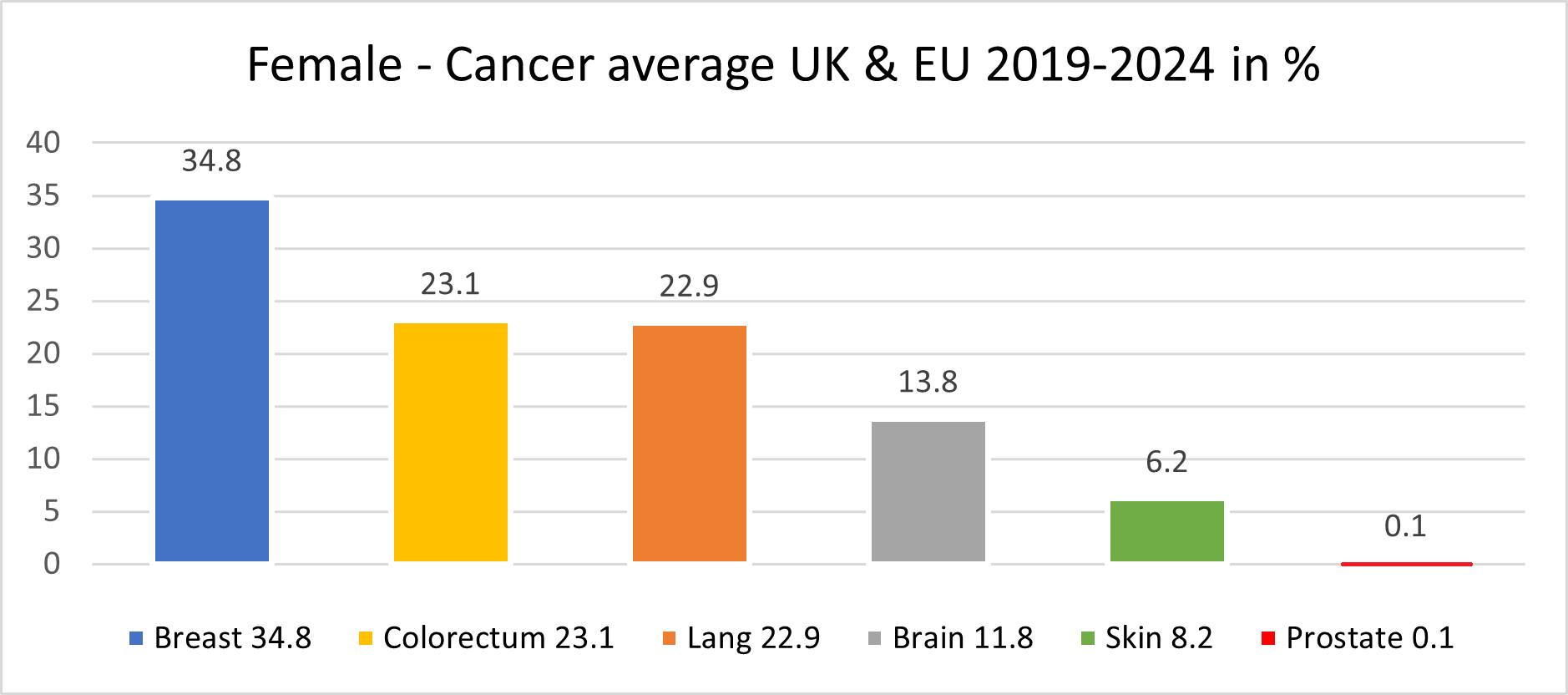
The female population in this period, some 390.1 million, recorded an average 2,398,547 new cancer cases per year; an ASR of 258.6 and a cumulative risk of 26.5%.
The top 3 most common cancers in females were Breast, Colorectum, and Lung cancer.
A significant point with cancer in the female population was the drop in lung cancer to 3rd place, with colorectum cancer overtaking the 2nd place.
Our mortality database is a collection of death registration data which includes cause of death information from member states; we use only the data which has been properly coded to the International Classification of Diseases (ICD).
What has also changed in recent years is the age of the death rate. This had declined over time in several countries due to life improvements, early diagnoses, medical advances, and a general reduction in risk factors like smoking and even drinking. However, there is a worrying emerging trend with rates of cancer in the population group aged up to 16.
This is rising well over expectations, especially in the United Kingdom, Spain and France.
PERIOD 2018 -2023
PROSTATE CANCER DATA
Prostate Cancer Data
Mortality in EU 2018/23: 37,922; Mortality in UK 2018/23: 19,885 (EU & UK Standard Treatments)
Result by Starting using our New medication/Treatment
(Testing period 2018-2023 all age groups):
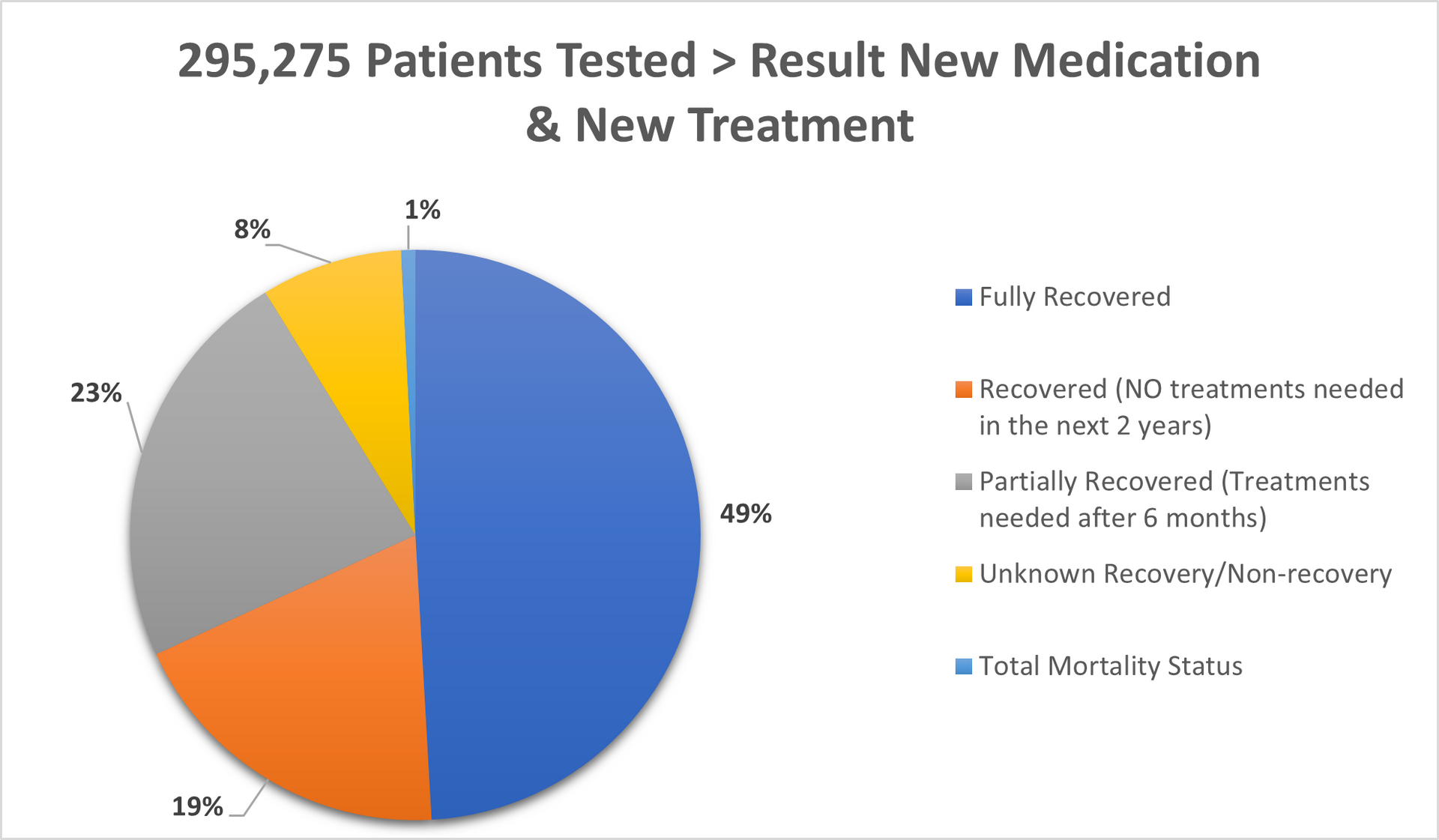
Tested patients in UK, Switzerland, Germany and Italy: 295,275
Fully Recovered (all risk levels): 49%
Recovered (No further treatments needed for period of next couple of years): 19%
Partially Recovered (Further treatments needed as precaution after 6months passed): 23%
Unknow Recovery/ Non-recovery: 8%
Deaths in Total: less than 1% (Mostly people age over 82).
REFERENCES TO THE DATA ABOVE:
Age Gap:
The youngest person was of 18 years of age
The oldest person was well over 88 years of age
Gender:
Female: Only 4 of 295,275 (Prostate cancer with female are very very rare)
Male: 295,271
- % of age group 18-25 was 4.2%
- % of age group 26-45 was 22.4%
- % of age group 46-65 was 30.8%
- % of age group 66-88 was 42.6%
Methods:
Old Methods meaning the standard methods used by hospital on daily basis for last minimum 5 years in EU and in the UK.
New Methods meaning our medication/treatment with which we came out after over 12 years of research and test.
New Methods combine meaning our medication/treatment combined in double parallel treatment > new medication and different way of treatment
Separate there are also results of our new medication/treatment combined with "old" methods however the final readings cannot be 100 percent accurate and cannot be as such used for whatever compares.
Mortality:
In the Europe 2018-2023 > 10.2%
In the United Kingdom 2018-2023 > 8.8%
With our medication/treatment in Europe & United Kingdom 2018-2023 > Less than 1%.
All patients being chosen randomly.
