PROSTATE CANCER - START YOUR TREATMENT NOW
THE BEST DOCTORS, THE BEST HOSPITALS, THE BEST MEDICATIONS and TREATMENTS
PROSTATE CANCER BASICS
Prostate cancer is a disease with a favourable prognosis, if this term can be ascribed to a malignant tumour. Like any cancer, it is characterized by infiltrative growth and metastases.
However, the tumour grows slowly and metastasizes later on.
Early diagnosis of prostate cancer is difficult to determine due to the lack of symptoms and late turnover of the patients. However, up to stage 3, the disease is well treatable when there are no distant metastases present.
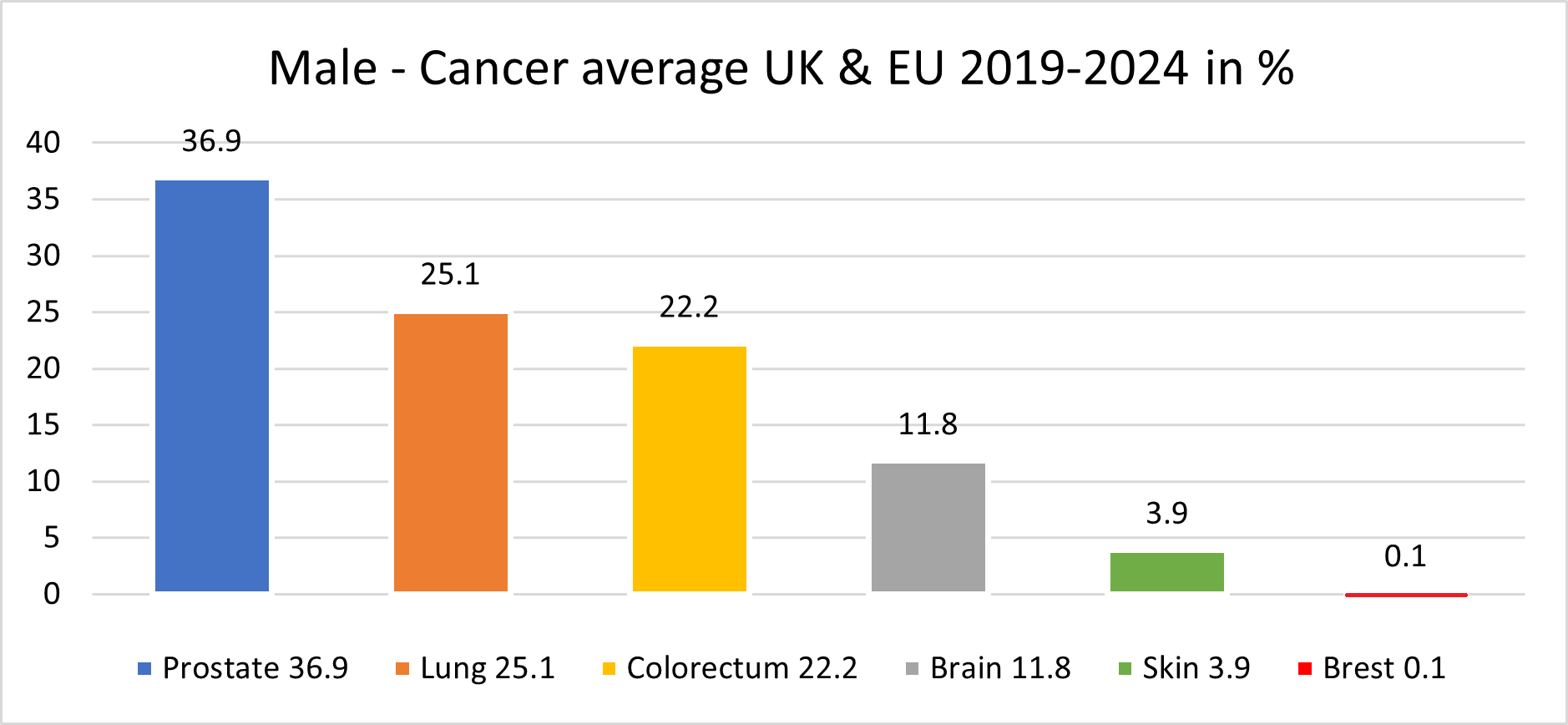
Because of the high prevalence among men, prostate cancer is considered the second most common oncological cause of death among males.
In quite a few Europe countries there are still in 1 male out of 40, prostate cancer causes death.
Make no mistake, with The Zdenko Kos Foundation our death rate is less than 1% doesn’t matter the stage as we are the only one who are having currently the best possible treatment for prostate cancer
Prostate cancer treatment by Zdenko Kos Foundation
combined with improved treatments methods.
Book Your Prostate Cancer Standard Treatment Here
STANDARD PROCEDURES IN EUROPE AND IN THE UNITED KINGDOM
ACTIVE SURVEILLANCE
Active surveillance
is often used to mean monitoring the cancer closely, with a plan to treat it if tests show it’s starting to grow more quickly. Usually, this approach includes doctor visits with a prostate-specific antigen (PSA) blood test about every 6 months and a digital rectal exam (DRE) about once a year.
Prostate biopsies and imaging tests may be done every 1 to 3 years as well. Exactly how often tests are done can be tailored to some extent, based on each man’s situation and preferences.
If test results change, you have to start with the treatment options to try to cure the cancer on as earlier possible stage.
Observation (watchful waiting)
is sometimes used to describe a less intense type of follow-up that includes fewer tests and that relies more on changes in a man’s symptoms to decide if treatment is needed. This is more likely to be a good option for men who are older and/or have other serious health problems.

CHEMOTHERAPY
Chemo drugs for prostate cancer are typically given into a vein (IV) as an infusion over a certain period of time. There are some drugs, which are given as a pill.
Sometimes, a slightly larger and sturdier IV might be put into a vein to give chemo.
These are known as central venous catheters (CVCs), central venous access devices (CVADs), or central lines.
They are used to put medicines, blood products, nutrients, or fluids right into your blood.
They can also be used to take out blood for testing. There are many kinds of CVCs available. The most common types are the port and the PICC line.
Chemotherapy is given in cycles, with each period of treatment followed by a rest period to give patient time to recover from the effects of the drugs.
Cycles are most often about 3 weeks long. The schedule varies depending on the drugs used.
Some drugs (the chemo) is given only on the first day of the cycle. With others, it is given for a few days in a row, or once a week.
Then, at the end of the cycle, the chemo schedule repeats to start the next cycle.
How long patient will be given chemo depends on how well it’s working and what side effects patient might have.

SURGERY
Radical prostatectomy
The main type of surgery for prostate cancer is a radical prostatectomy. In this operation, the surgeon (urologist) removes the entire prostate gland plus some of the tissue around it, including the seminal vesicles. Sometimes nearby lymph nodes are removed as well.
There are 2 main ways a surgeon can do a radical prostatectomy:
- Open prostatectomy:
the surgeon operates through a single long skin incision (cut) to remove the prostate and nearby tissues.
- Laparoscopic prostatectomy:
the surgeon makes several smaller incisions and uses long, thin surgical tools to remove the prostate and nearby tissues.
Most often, the surgeon sits at a control panel to precisely move robotic arms that hold the tools (known as a robot-assisted prostatectomy or robotic prostatectomy).
The operation can also be done with the surgeon holding the tools directly, although this is less common.
With either type of operation, if there’s a reasonable chance the cancer might have spread to nearby lymph nodes (based on your PSA level, prostate biopsy results, and other factors), the surgeon may first remove some of these lymph nodes (known as a pelvic lymph node dissection).
The nodes are sent to the lab to be looked at right away for cancer cells. If cancer cells are found in any of the nodes, the surgeon might not continue with the surgery.
This is because it’s unlikely that the cancer can be cured with surgery, and removing the prostate could lead to serious side effects.
OPEN PROSTATECTOMY I
Radical retropubic prostatectomy
For this operation, the surgeon makes an incision (cut) in your lower abdomen, from the belly button down to the pubic bone, as shown in the picture below.
You will either be under general anaesthesia (asleep) or be given spinal or epidural anaesthesia (numbing the lower half of the body) along with sedation during the surgery.
After the prostate and nearby structures have been removed, and while you are still under anaesthesia, a catheter (thin, flexible tube) will be put in your penis to help drain your bladder.
The catheter will usually stay in place for 1 to 2 weeks while you heal. You will be able to urinate on your own after the catheter is removed.
You will probably stay in the hospital for a few days after the surgery, and your activities will be limited for several weeks.
OPEN PROSTATECTOMY II
Radical perineal prostatectomy
In this open operation, the surgeon makes the cut (incision) in the skin between the anus and scrotum (the perineum), as shown in the picture above.
This approach is used less often because it’s more likely to lead to erection problems and because the nearby lymph nodes can’t be removed during the operation. But it is often a shorter operation, and it may result in less pain and an easier recovery than a retropubic prostatectomy.
This approach might be an option if you aren’t concerned about erections and if you don’t need lymph nodes removed. It also might be used if you have other medical conditions that might make retropubic surgery difficult for you. It is just as likely to cure prostate cancer as the retropubic approach if done correctly.
After the surgery, and while you are still under anaesthesia, a catheter will be put in your penis to help drain your bladder. The catheter usually stays in place for 1 to 2 weeks while you are healing. You will be able to urinate on your own after the catheter is removed.
You will probably stay in the hospital for a few days after the surgery, and your activities will be limited for several weeks.
PROSTATE CANCER STANDARD and IMPROVED TREATMENTS
Prostate cancer is one of the most common types of cancer in men, most often affecting middle-aged and elderly men. Prostate cancer develops slowly and may progress for years without any symptoms; the initial manifestations of the disease appear at stage 2 or later. The primary diagnostic measure for suspected prostate cancer is a PSA blood test. If the result is unsatisfactory, the team of specialists from The Zdenko Kos Foundation and doctors from the hospital where you will be admitted will additionally perform magnetic resonance imaging (MRI) and a transperineally MRI-guided prostate biopsy.
Most clinics perform a transrectal puncture biopsy of the prostate gland. However, it provides doctors with an accurate diagnosis in only 30-35% of cases, so the medical team prefers a transperineally MRI-guided biopsy. With this method, the reliability of diagnostic data reaches 100%. This approach allows the patient to avoid unnecessary invasive procedures.
To detect prostate cancer metastases, the department's doctors use Ga-68 PSMA PET/CT instead of a CT scan and bone scintigraphy, which not so long ago were considered the standard methods of prostate cancer staging. It has already been proven that, among all diagnostic methods, Ga-68 PSMA PET/CT allows for the most accurate detection of prostate cancer metastases in any location.
Standard and innovative prostate cancer treatments are divided in three treatment groups:
- Treatment of prostate cancer and bladder cancer
- Irreversible electroporation (IRE)
- Combination treatment with irreversible electroporation and electrochemotherapy (IRECT)
- Combination treatment with irreversible electroporation and immunotherapy
- Photodynamic therapy (PDT)
- Combination treatment with photodynamic therapy and immunotherapy
- Treatment of benign prostatic hyperplasia
- GreenLight laser therapy
- Rezum water vapor therapy
- Other treatment methods
As for the treatment of prostate cancer, the Zdenko Kos Foundation is proud to offer patients innovative and minimally traumatic methods to combat oncology. The gold standard of prostate cancer treatment is a prostatectomy (prostate removal surgery). For patients with unresectable tumours, doctors offer irradiation. The department's doctors use revolutionary new types of treatment, the effectiveness of which is comparable to prostatectomy and radiation therapy. At the same time, these new treatment procedures help the doctors eliminate the development of complications after the completion of therapy, namely erectile dysfunction and urinary incontinence, which are almost unavoidable with classic prostatectomy or radiation therapy.
NanoKnife irreversible electroporation (IRE):
Is a promising low-traumatic method for prostate cancer treatment, and the medical team working with The Zdenko Kos Foundation have vast experience in its use. The essence of the method consists in the selective ablation (destruction) of cancer cells by the powerful electric field of the NanoKnife device.
The medical team specialists at different hospital working with The Zdenko Kos Foundation around the Europe have successfully performed more than 4,200 IRE procedures. This method provides excellent results and helps patients with advanced stages of prostate cancer.
Irreversible electroporation is performed under general anaesthesia, does not require extensive tissue incisions, and is more than just tolerated. Unlike prostatectomy and radiatiotherapy, IRE practically eliminates the risk of erectile dysfunction. Also, during the entire period of application of this treatment method, none of the patients developed postoperative urinary incontinence. Normal hospital stay for IRE treatment is only 3 days.
Irreversible electroporation and electrochemotherapy (IRECT):
for patients with prostate cancer. In these cases, the effect of the IRE procedure is enhanced by simultaneously applying electrical current and low-dose chemotherapy to cancer cells. Irreversible electroporation increases the permeability of the cell wall, which allows chemotherapy drugs to easily penetrate cancer cells and effectively destroy them. The combination IRECT method may be indicated for patients with high-grade tumours, patients with cancer that has invaded the rectum or bladder wall, and patients with complex focal prostate cancer recurrences after surgery, HIFU, or radiation therapy.
Irreversible electroporation with immunotherapy treatment:
In this case, the effect of IRE is enhanced by activating the patient's anti-cancer immunity. The immune system is "trained" to recognize cancer cells by antigens located on their surface. During irreversible electroporation, tumour antigens are released in large quantities, and it is easier for the immune system to recognize them, subsequently destroying the cancer cells.
Photodynamic therapy (PDT):
Is regularly performed for the treatment of prostate cancer and bladder cancer. This treatment uses photosensitizers and light sources of a certain length. The photosensitizer accumulates in the cancer cells and does not threaten healthy tissues. After the accumulation of the photosensitizer, the tumour is irradiated with light of a certain wavelength. As a result, chemical processes are launched that lead to the formation of active oxygen radicals. Oxygen radicals are toxic to cancer cells, so they can easily destroy them. In addition, PDT triggers an anti-cancer immune response by causing dying tumour cells to release specific antigens that the patient's immune system recognizes, resembling a vaccination mechanism. Tumour antigens allow the natural killer cells of the immune system to recognize and eliminate tumour cells in the patient's body.
Benign prostatic hyperplasia - GreenLight laser therapy and the Rezum procedure:
If untreated, the disease causes serious bladder voiding dysfunction, frequent nocturnal urination, and elevated PSA levels in the blood, which in turn potentially threatens the development of prostate cancer.
Minimally invasive procedures for prostate adenoma treatment are GreenLight laser therapy and the Rezum procedure.
The hospital stay for such treatments is 1-2 days.
Unlike the standard transurethral resection of the prostate, GreenLight and Rezum are bloodless procedures. In addition, innovative GreenLight and Rezum treatments eliminate the risk of developing erectile dysfunction and urinary incontinence.
LAPAROSCOPIC PROSTATECTOMY (Include Robotic Prostatectomy)
Laparoscopic prostatectomy (including robotic prostatectomy)
Laparoscopic surgery
is done through several small incisions in the abdomen, rather than one large incision. The surgeon inserts a laparoscope, which is a long, thin tube with a light and tiny video camera on the end, through one of the openings so they can see inside the body. Long, thin surgery instruments are then inserted through the other incisions to perform the operation.
This approach to prostatectomy (particularly robotic prostatectomy) has become much more common in recent years.
Laparoscopic radical prostatectomy
For a laparoscopic radical prostatectomy (LRP), the surgeon holds the handles of the long instruments directly to manoeuvre them inside the belly and remove the prostate. This approach is not used as often as robotic prostatectomy.
Robotic prostatectomy
This approach, also known as robotic-assisted laparoscopic radical prostatectomy or robot-assisted prostatectomy, is the most common way prostatectomy is done in the United States.
This operation is done using a robotic system. The surgeon sits at a control panel in the operating room and moves robotic arms to operate through several small incisions, usually in the patient’s abdomen (although it can also be done with a perineal approach). The robotic system helps the surgeon move the instruments more precisely than if they were holding the laparoscopic tools directly in their hands.
ROBOTIC v OPEN RADICAL PROSTATECTOMY (Things you should know)
Robotic prostatectomy is the most common surgery to treat prostate cancer in quite a few countries around the Europe. That is largely because this operation has some short-term advantages over open radical prostatectomy. Normally results in:
- Less blood loss during the operation
- Less pain after the operation
- A shorter hospital stays
- A quicker recovery time
- Less time the urinary catheter needs to stay in place
- A lower risk of some rare but potentially serious side effects
However, the results of robotic and open prostatectomy seem to be about the same when it comes to the long-term side effects that many men are most concerned about, including erection problems and trouble holding urine (incontinence). (These are described below.)
There also doesn’t appear to be much difference between robotic and open prostatectomy when it comes to long-term outcomes. That is, studies haven’t shown that either approach is clearly better than the other when it comes to how likely the cancer is to return after surgery or how likely a man is to die from prostate cancer. Both approaches generally result in good outcomes when done by experienced surgeons.
In some instances, there might be clear reasons to favour one approach over the other.
Make no mistake, doesn’t matter which prostatectomy approach you choose, the biggest factor in the success of your surgery is likely to be the experience and skill of your surgeon. Therefore, it’s very important to go with an experienced surgeon whom you’re comfortable with and whom you can trust.
Risks of prostatectomy
The risks with any type of radical prostatectomy are much like those of any major surgery. Problems during or shortly after the operation can include:
- Reactions to anaesthesia
- Bleeding from the surgery
- Blood clots in the legs or lungs
- Damage to nearby organs
- Infections at the surgery site
- Rarely, part of the intestine might be injured during surgery, which could lead to infections in the abdomen and might require more surgery to fix. Injuries to the intestines are more common with laparoscopic and robotic surgeries than with the open approach.
If lymph nodes are removed, a collection of lymph fluid (called a lymphocele) can form and may need to be drained.
Your risks depend, in part, on your overall health, your age, and the skill of your surgical team.
Side effects of prostatectomy
The major possible side effects of radical prostatectomy are:
- Urinary incontinence (being unable to control urine)
- Erectile dysfunction (problems getting or keeping erections)
- These side effects can also occur with some other forms of prostate cancer treatment.
- Other side effects are also possible (see below).
Urinary incontinence
You may not be able to control your urine, or you may have leakage or dribbling after your surgery. Being incontinent can affect you not only physically, but also emotionally and socially. These are the major types of incontinence:
Men with stress incontinence might leak urine when they cough, laugh, sneeze, or exercise. Stress incontinence is the most common type after prostate surgery. It’s usually caused by problems with the valve that keeps urine in the bladder (the bladder sphincter). Prostate cancer treatments can damage this valve or the nerves that keep the valve working.
Men with overflow incontinence have trouble emptying their bladder. They take a long time to urinate and have a dribbling stream with little force. Overflow incontinence is usually caused by blockage or narrowing of the bladder outlet by scar tissue.
Men with urge incontinence have a sudden need to urinate. This happens when the bladder becomes too sensitive to stretching as it fills with urine.
Rarely after surgery, men lose all ability to control their urine. This is called continuous incontinence.
After surgery for prostate cancer, bladder control usually improves slowly over several weeks or months. But doctors can’t predict for sure how any man will be affected. In general, older men tend to have more incontinence problems than younger men. Large cancer centers, where prostate surgery is done often and surgeons have a lot of experience, generally report fewer problems with incontinence.
Incontinence can be treated. Even if your incontinence can’t be corrected completely, it can still be helped. To learn about managing and living with incontinence, see Bladder and Bowel Incontinence.
Erectile dysfunction (impotence)
This means you can’t get an erection sufficient for sexual penetration.
Erections are controlled by 2 tiny bundles of nerves that run along either side of the prostate. If you can have erections before surgery, the surgeon will try not to injure these nerves during the prostatectomy. This is known as a nerve-sparing approach. But if the cancer is growing into or very close to the nerves, the surgeon will need to remove them.
If both nerves are removed, you won’t be able to have spontaneous erections, but you might still be able to have erections using some of the aids described below. If the nerves on only one side are removed, you might still have erections, but the chance is lower than if neither were removed. If neither nerve bundle is removed, you might have normal erections at some point after surgery.
Your ability to have an erection after surgery depends on your age, your ability to get an erection before the operation, and whether the nerves were cut. Most men will probably have at least some loss of ability to have an erection, but the younger you are, the less likely you are to be seriously affected.
Surgeons who do many prostatectomies tend to report lower rates of erection problems among their patients than those who do the surgery less often. A wide range of rates have been reported in the medical literature, but each man’s situation is different, so the best way to get an idea of your chances for recovering erections is to ask about your doctor’s success rates and what the outcome is likely to be in your case.
If your ability to have erections does return after surgery, it often returns slowly. In fact, it can take from a few months to 2 or more years. During the first few months, you will probably not be able to have a spontaneous erection, so you may need to use medicines or other treatments.
Many doctors feel that regaining potency is helped along by trying to get an erection as soon as possible once the body has had a chance to heal (usually several weeks after the operation). Some doctors call this penile rehabilitation. Medicines (see below) may be helpful at this time, although it’s not clear if they work better if taken daily or just on an as-needed basis. Be sure to talk to your doctor about your situation.
Options for treating erectile dysfunction:
Phosphodiesterase-5 (PDE5) inhibitors, such as sildenafil (Viagra), vardenafil (Levitra), tadalafil (Cialis), and avanafil (Stendra), are pills that can help with erections. These drugs won’t work if both nerves that control erections have been damaged or removed. Common side effects of these drugs include headache, flushing (skin becoming red and feeling warm), upset stomach, light sensitivity, and runny or stuffy nose. Rarely, these drugs can cause vision problems, possibly even blindness. Some other drugs such as nitrates, which are used to treat heart disease, can cause problems if you are taking a PDE5 inhibitor, so be sure your doctor knows what medicines you take.
Alprostadil is a man-made version of prostaglandin E1, a substance naturally made in the body that can produce erections. It can be injected almost painlessly into the base of the penis 5 to 10 minutes before intercourse or placed into the tip of the penis as a suppository. You can even increase the dosage to prolong the erection. You might have side effects, such as pain, dizziness, and prolonged erection, but they are not usually serious.
Vacuum devices are another option to create an erection. These are clear, plastic tubes connected to pumps that are placed over the penis. The pump sucks the air out of the tube, which draws blood into the penis to produce an erection. After the device is removed, the erection is maintained by placing an elastic ring around the base of the penis, which keeps the blood from draining out. The ring is then removed after sex.
Penile implants might restore your ability to have erections if other methods don’t help. An operation is needed to put them inside the penis. There are several types of penile implants, including those using silicone rods or inflatable devices.
For more on coping with erection problems and other sexuality issues, see Sexual Side Effects.
Changes in orgasm
After surgery, the sensation of orgasm should still be pleasurable, but there is no ejaculation of semen – the orgasm is “dry.” This is because the glands that made most of the fluid for semen (the seminal vesicles and prostate) were removed during the prostatectomy, and the pathways used by sperm (the vas deferens) were cut. In some men, orgasms might become less intense. Less often, men report pain with orgasm.
Loss of fertility
During a radical prostatectomy, the surgeon cuts the vas deferens, which are the pathways between the testicles (where sperm are made) and the urethra (through which sperm leave the body). Your testicles will still make sperm, but they can’t leave the body as a part of the ejaculate. This means that a man can no longer father a child the natural way.
Often, this is not an issue, as men with prostate cancer tend to be older. But if it is a concern for you, you might want to ask your doctor about “banking” your sperm before the operation. To learn more, see Fertility Problems.
Lymphedema
This is a rare but possible complication of removing many of the lymph nodes around the prostate. Lymph nodes normally provide a way for fluid to return to the heart from all areas of the body. When nodes are removed, fluid can collect in the legs or genital region over time, causing swelling and pain.
Lymphedema can usually be treated with physical therapy, although it may not go away completely. You can learn more on our lymphedema page.
Change in penis length
A possible effect of surgery is a small decrease in penis length. This can result from a shortening of the urethra when a portion of it is removed along with the prostate.
Inguinal hernia
A prostatectomy increases a man’s chances of developing an inguinal (groin) hernia in the future.
Transurethral resection of the prostate (TURP)
This operation is more often used to treat men with non-cancerous enlargement of the prostate called benign prostatic hyperplasia (BPH). But it is also sometimes used in men with advanced prostate cancer to help relieve symptoms, such as trouble urinating. (It is not used to try to cure the cancer.)
During this operation, the surgeon removes the inner part of the prostate gland that surrounds the urethra (the tube through which urine leaves the bladder). The skin is not cut with this surgery. An instrument called a resectoscope is passed through the tip of the penis and into the urethra to the level of the prostate. Once it’s in place, either electricity is passed through a wire to heat it or a laser is used to cut or vaporize the tissue.
This operation is done with either spinal anaesthesia (which numbs the lower half of your body) or general anaesthesia (where you are in a deep sleep), and it usually takes about an hour.
After surgery, a catheter (thin, flexible tube) is inserted through the penis and into the bladder. It remains in place for about a day to help urine drain while the prostate heals. You can usually leave the hospital after 1 to 2 days and return to normal activities in 1 to 2 weeks.
You will probably have some blood in your urine after surgery.
Other possible side effects from TURP include infection and any risks that come with the type of anaesthesia used.
Orchiectomy (castration)
In this operation, the surgeon removes the testicles, where most of the androgens (male hormones) are made. Although this is a type of surgery, its main effect is as a form of hormone therapy. To learn more about this operation, see Hormone Therapy for Prostate Cancer.

PRICES FOR PROSTATE CANCER STAGE 4
Prostate cancer Standard and Improved treatment Price List:
- Prostate cancer diagnostics £4,800
- Prostate cancer standard treatment full course £46,600
- Prostate cancer innovative methods full course £19,200
- Oncological rehabilitation £0.00 if booked and admitted with The Zdenko Kos Foundation.
The above figures represent ¼ of the price, the balance of ¾ of the original price contributed and covered by The Zdenko Kos Foundation.
YOUR QUESTIONS ANSWERED
What is included in the treatment plan and pathway?
Following receipt of your initial submission and supporting documents (clinical letters, imaging, test results), you will be asked to select your preferred hospital from our list:
- You will then be advised of available admission dates for your initial two day stay
- On admission you will have a full diagnostic review, with all tests and investigations completed within 24 hours of your arrival.
- Your face-to-face consultation will then take place with the appropriate specialist Consultant and resident Doctor. The treatment plan will be presented for discussion and agreement; if the first proposal is not acceptable to you, an alternative treatment plan will be offered.
- Treatment can commence that day; treatment may include chemotherapy, radiotherapy, surgery and other therapies.
- Dependent on your treatment pathway you will either stay in hospital or you will be discharged and advised when you need to return.
- Hospital visits can be required every 2-3 weeks; the fixed fee includes all hospital visit and treatments for up to one year
Can I choose the hospital for my treatment?
Yes, you can select the hospital you would like to be during your treatment, however, keep in mind that that particular hospital must have a department and wards for the kind of profile of your medical issue. When the patients identify where they would like to have their treatment, they must have in mind the remoteness from the airports, main road and main railways in cases of any emergencies.
We’ll give our recommendation which is based on a long experience and a profound analysis of all criteria necessary for the quality of medical the patients are looking for.
How much does treatment cost?
When you book your treatment with us you will get fix figure of which you are paying just ¼ of original cost only, the balance of ¾ contributed and paid by Zdenko Kos Foundation.
Costs for hospitals are also fixed for entire year, therefore, if you are having treatment over one year, the hospital costs might changed. Once you make the payment for the hospital (eg. for one year) you have hospital free of any charges doesn't matter how many times and days per year you spent in the hospital, doesn't matter how many times you are booked and discharged from the hospital.
What is the cost of your services
Depending on the duration of the medical program the cost in every hospital doesn't matter, the country may vary - but not when you are booking with us. Our prices are fixed doesn't matter what we may find once eg. surgery or treatment start. All the costs of our services are significantly lower, up to 80% (depending on treatment) that you will have to pay either through your health system in your country or when organizing the program on your own. There are several reasons for it: The hospitals provided by us have special contract agreements to have fixed rates with discounts for the entire year. There are no overstated rates. You and the hospital you will be having treatment are insured specially from unforeseen expenses eg. possible complications.
With whom will I conclude the contract?
You must book with us, and you will complete the contract with us - The Zdenko Kos Foundation. It is a contract on the organization of a medical trip and provision of services. The protocol is very clear:
[1] You have to make the booking with us online on this web site (see the page with the booking box) for the treatment you are after where we are strongly suggest to give us as much data and images of your medical condition to date that we can contact you directly with our doctors, consultants and other medical staff for the treatment you would like to have.
[2] Once booking is completed, you will receive automated mail for the payment to be made. You have to make the payment in full for the treatment you would like to have in maximum 24 hours after the booking. With making the payment you start ball rolling.
[3] Being admitted to the hospital, you will conclude a direct contract with us for the provision of medical services.
{4} Once payment made you will get direct link to the doctor and counsaltant to discuss your case face-to-face via What's Up or other such service provider available to both parties depend on your locatition.
Why should I pay you, but not the hospital?
Firstly, unlike many intermediary firms and portals, we do not take from hospitals a percentage of the medical service cost because we have contract agreement not just with hospitals but also with doctors, consultants and other medical professional in each hospital we are working with.
Secondly, we are covering ¾ of costs for your procedure not to mention that your procedure-treatment will be fully insured up to £250,000 (for one year treatment) and automatically up to £500,000 (for 2-5 years treatment). The Zdenko Kos Foundation cover the hospital insurance seperately during your treatment if there may come to unforseen complication during the treatment.
Finally, as we are registered as charity, we remain independent in choosing a medical facility and work exclusively for the benefit of the patient. Any type of payment for sending a patient to the hospital is prohibited by law, since it contradicts medical ethics.
At what point do the services become paid?
The services for the organization of treatment become paid from the moment you made your medical treatment booking online and make the payment in full. Once this done, pre-treatment consultation will take the place following the initial examination (hospitalization).
Can I contact the hospital directly?
Yes, of course, you can also contact the hospital on your own. You should choose the hospital and the attending doctor, write an email to the chief doctor with a description of your case in English, ask him/her about the possibility of undergoing treatment in the hospital and the approximate cost of staying there. If you have received the consent of the hospital and you are satisfied with the price for the hospital (please specify that it must be the price for one year doesn’t matter on number of admissions and discharges and transfer an advance payment to us on our account. Once full payment is received, we will negotiate special terms with the hospital you select on your own that they will be aware of what and how many procedures they have to have in mind and secure at any time free bad in ward. If you are coming from a non-EU country write an email to the secretary of the hospital with a request to send an invitation for a visa. Please note that the invitation should come from the chief doctor, but not from the hospital's international department. After that you should on your own get a visa for medical treatment abroad, agree with the secretary of the chief physician on the date of the initial examination (hospitalization), translate medical records of local physicians into German or English (depending on the chosen country for treatment), book a hotel, prepare a transfer from the airport and find for yourself an interpreter for communication with the medical staff.
All these activities are not needed in case you are booking with us and you are choosing a hospital we would recommend. If you book with us, we will deal with your visa (if you are coming from a non-EU country), we will book you a hotel, and do all that is necessary to get you started with your treatment.
Shall I pay for a consultation?
A consultation before the treatment as well as long-distance consultation (if you are not from EU countries) is provided free except when you are returning to your home address and it is necessary to study CT or MRI images as the specialist gives an official consultation with a written opinion.
If you are not from EU countries it is imperative to translate epicurises and medical records from domestic doctors into English.
If you opt for our services for the organization of treatment with us, there is no need to translate the medical records. This will be done by qualified specialists.
What happens, if I refuse from the treatment?
If you refuse from the treatment you will get a refund of the advance payment.
The expenses for all what has been done to that moment will be deducted acordingly.
Is it possible to postpone the treatment?
Yes, it is. In case of an advance postponement (more than 48 hours before the start of the treatment), the treatment cost will not be changed, and will be deleyed till as per your request. If you intend to postpone the treatment, you must do so on written only. There may be some additional cost for consultation or pre-treatment appointment, depend on the lenght from the initial day of treatment till the day you want to be.
What security and guarantees do I have?
When booking the treatment with us all medical treatment are fully insured against possible complications and unforeseen contingencies. The additional treatment costs will be covered by the insurance covered and paid by The Zdenko Kos Foundation.
How is my personal data managed?
The Kos Foundation is a Data Controller therefore rest assured that your personal data and all material you submit over our link along with all medical history with us will be protected according to current regulations and legislation, using advanced security technologies. Medical history will not be disclosed to any 3rd party even to your GP without your special written permission.
Check list for inpatient and outpatient
When you pack your bag for your hospital stay, the following things should not be missing:
For your record
- Referral certificate from the general practitioner or specialist
- Health insurance card
For your treatment
- Medicines in original packaging that you take at home
- Current preliminary findings, such as X-rays, CT/MRI, ECG or EEG, blood tests, etc.
- Doctor's Letters
- If available, living will and power of attorney
- If available: allergy passport, vaccination certificate, X-ray passport, diabetic card, blood group card
For your stay
- Your aids (e.g. wheelchair, walker, walking stick, glasses, hearing aid)
- Comfortable clothing
- Towels
- Cosmetics and personal care products
- To pass the time: books, magazines, MP3 player with headphones
- Contact details of relatives and friends
Please be aware:
When you get your inpatient admission appointment, please clarify whether you have to appear fasting on the day of admission.
Valuables
If possible, please do not bring any valuables with you, as you are liable for losses. For indispensable valuables, e.g. Your watch or wallet, you will find a small safe deposit box in the closet of your patient room in the Surgery I Dermatology and in the Psychosomatics department. In internal medicine, there is a dispensing point.
How are the visiting hours regulated?
Visitors are not only welcome to us but are also of huge importance for our patients!
Doesn’t matter with which hospital we are working with you are booking there are variable visiting hours, as well as special visiting hours which are not for regular patients visits. Once you are admitted the care team will give you all the details about visiting hours. There are also alternative that your partner (husband/wife) stay with you during the treatment. Such accommodation is available nearly in all hospitals we are working with. For such accommodation additional charges applies.
There are separate visiting hours for intensive care units while parents of young patients in the children's area have unlimited visiting hours.
Visitors are asked to be considerate of patients and fellow patients. If necessary, the nursing staff of that hospital where you are staying, will point out the necessary rest periods for patients who have just undergone surgery
Where can I reach pastoral care?
All hospitals we are working with offer pastoral care for at the Protestant and Catholic hospital chaplaincy for patients and relatives. For all other religions you will be informed by the care team at that particular hospital on the day of your admission.
What help and counselling services are available?
Doesn’t matter which hospital we are working with you choose, you will be given supports with various counselling services and support services, such as the Social Counselling Service, Psychosomatic consultation service, Special offers for cancer patients, Clinic chaplaincy, Services of other religious communities, Art therapy, Self-help, Hospice and much more.
How can I contact social services?
The Social Counselling Service can advise you on topics such as rehabilitation, post-discharge care, social law, psychosocial care and many other matters. You will get special overview with information and contact details from consultant and care team in the hospital where you start your treatment.
Inpatient stay: How is admission made?
Registration and admission for an inpatient stay
If you have made an appointment for an inpatient stay in cooperation with The Zdenko Kos Foundation, you will first be "admitted" to hospital of your choice upon arrival. This means that we record your data and inform you about your hospital stay.
Please ask exactly where you should travel when making an appointment. The Zdenko Kos Foundation has several locations and consists of many individual clinics.
An overview of the parking facilities at the clinic locations will be provided once you identify the hospital you would like to be admitted to.
When you get your inpatient admission appointment, please clarify whether you have to appear fasting on the day of admission.
What should be considered when discharging?
Your attending physician has decided that you will be discharged from the hospital. This means that you will either be discharged directly to your home or still need follow-up treatment, which will be carried out on an outpatient or inpatient basis in another clinic or rehabilitation facility. For both situations, you will get full information before discharged date.
What do the General Terms and Conditions of Contract regulate?
Accepting services of The Zdenko Kos Foundation, you are not accepting just our Terms & Conditions but also for the period of your entire treatment or stay doesn’t matter which hospital we are working with, the hospital GTCs and the house rules of that hospital in their respective valid versions which you can see and read on hospital websites directly.